Cancer-killing T cells enhanced by engineered bacteria
Posted: 20 October 2023 | Drug Target Review | No comments yet
Bacteria programmed to paint targets on solid tumours for T cells to see eliminates the need for specific antigens.
Scientists have successfully used chimeric antigen receptor (CAR) T cells for several years to target specific antigens on blood cells as a cure for leukaemia and lymphoma patients. However, solid tumours like breast and colon cancers have been more challenging to treat because solid tumours contain a mix of cells that display different antigens on their surface that are often shared with healthy body cells. Therefore, detecting a consistent and safe target has interfered with the success of most CAR-T cell therapy for solid tumours.
Engineering bacteria
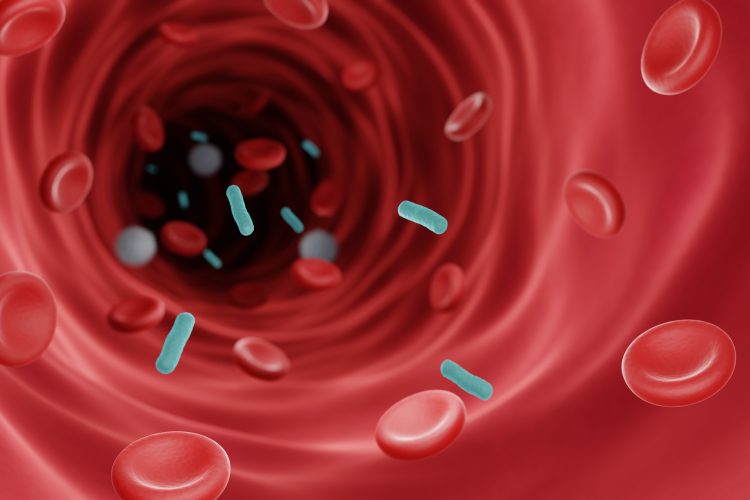
Published in Science, synthetic biologists at Columbia University School of Engineering and Applied Science reported a novel approach to targeting tumours: engineering tumour-colonising bacteria (probiotics) to produce synthetic targets in tumours that direct CAR-T cells to destroy the newly highlighted cancer cells.
Dr Tal Danino, Associate Professor of Biomedical Engineering and lead author, said: “Our probiotic platform enables CAR-T cells to attack a broad range of tumour types.” He added: “Traditional CAR-T therapies have relied on targeting natural tumour antigens. This is the first example of pairing engineered T cells with engineered bacteria to deliver synthetic antigens safely, systemically, and effectively to solid tumours. This could have a significant impact on the treatment of many cancers.”
Painting targets
Danino’s lab has created a universal CAR-T cell that attacks a universal antigen, by programming the tumour-seeking bacteria to paint solid tumours with a synthetic marker that the CAR-T cells can recognize. With more refinements the researchers expect that this will enable any solid tumour type to be treated without the need to identify a specific antigen. This escapes the need to produce a custom CAR-T cell product for each patient and each cancer type.
ProCAR
The probiotic-guided CAR-T cell (ProCAR) platform is the first time that scientists have both successfully combined engineered probiotics with CAR-T cells and have demonstrated the first evidence of CARs responding to synthetic antigens produced directly within the tumour.
Rosa Vincent, the study’s co-lead author and PhD student working in Danino’s lab, said: “Combining the advantages of tumour-homing bacteria and CAR-T cells provides a new strategy for tumour recognition, and this builds the foundation for engineered communities of living therapies.” She continued: “We chose to bridge the individual limitations of these two cell therapies by combining the best features of each – using bacteria to place the targets, and T cells to destroy the malignant cells.”
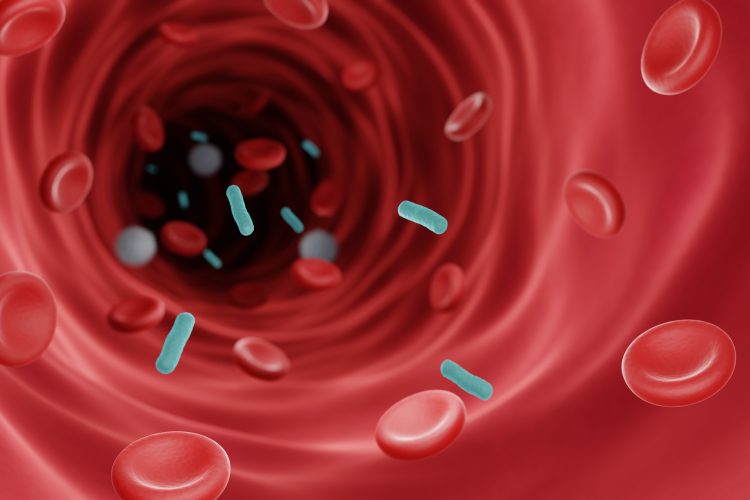
Tumour-killing functions enhanced
The ProCAR platform has proven to be safe and effective across multiple models of human and mouse cancers in both immunocompromised and immune-healthy mice. The study shows that human T cells especially benefit from the presence of immunostimulatory bacteria within the tumour, as their tumour-killing functions are further enhanced.
“Overall, our ProCAR platform represents a new strategy for enhancing the effectiveness of CAR-T cell therapy in solid tumours,” said Danino. “While we’re still in the research phase, it could open up new avenues for cancer therapy.”
This work was part of an ongoing collaboration with the laboratory of Nicholas Arpaia, Assistant Professor of Microbiology and Immunology at Columbia’s Vagelos College of Physicians and Surgeons. Previously, the team has developed bacteria that deliver immunotherapy payloads together. The researchers continue to refine their work which offers promise for clinical trials.