Developing an effective vaccine for herpes simplex virus
Posted: 13 February 2024 | Drug Target Review | No comments yet
Researchers have identified key differences between HSV-1 and HSV-2 and have developed monoclonal antibodies that could treat neonatal infections.
Researchers from Dartmouth’s Geisel School of Medicine and Thayer School of Engineering have provided new insights into how antibodies function when fighting herpes simplex virus (HSV) infections, which could result in novel treatments for neonatal herpes.
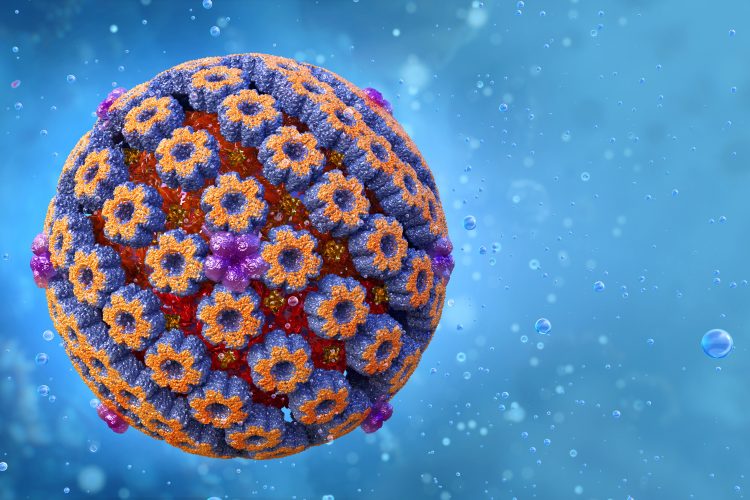
Herpes simplex virus infections are common and usually affect the skin and the nervous system. They are caused by two related but distinct viruses: type 1 (HSV-1) which more commonly causes infections around the mouth and occurs in up to 80 to 90 percent of older adults, and type 2 (HSV-2) which more commonly causes genital infections and can be found in 20 to 30 percent of adults.
These viruses often lay dormant in the body and typically do not pose serious health risks, but HSV can be dangerous for those with weak immune systems as it can cause corneal blindness and brain infections. Also, it may have an association with neurodegeneration and Alzheimer’s disease. Neonatal herpes simplex virus infection is one of the deadliest neonatal infections, as severe infections can spread to internal organs and the brain.
Co-corresponding author Dr David Leib, chair and professor of microbiology and immunology at Geisel, explained: “Despite three decades of trying, the scientific community has been unable to develop an effective vaccine against herpes, and I think the main issue has been that we haven’t fully understood what we need, in terms of antibodies and their specific functions, to protect against this disease.”
Dr Leib partnered with Dr Margaret Ackerman, professor of engineering at Thayer and other corresponding author on this study, and supervised Matthew Slein, PhD candidate in both of their labs, and Iara Backes, a PhD student at Geisel. In their experiments, the team used a neonatal mouse model to mimic human neonatal infections and engineered antibodies with different properties to explore how they mediate protection.
Dr Leib commented on Slein and Iara’s discovery: “It’s not just the neutralising capability of antibodies, that is, their ability to bind directly to the virus and prevent it from entering the cell, that is important. Effector functions, which allow the antibodies to interface with other parts of the immune system, also play a critical role—one that has been largely overlooked in the past.”
Slein and Backes also identified crucial differences between HSV-1 and HSV-2 infections, finding that each requires different antibody properties for optimal protection. Their results notably point to an improved way to design vaccines and may help to explain why many vaccine candidates have failed to be protective in prior clinical trials.
Dr Leib added: “Another important aspect of the work that Matt and Iara have done is that we now have some really good monoclonal antibodies that we’ve made in the lab that could potentially be used directly as a medication to treat acute neonatal herpes infections, which are life-threatening to newborns.”
He concluded: “Monoclonal antibodies have been used to treat cancer and other diseases and show promise as a therapy for infectious disease…This would be a wonderful development, as antiviral drugs like acyclovir have only proven to be partially effective in treating these very sick kids.”
This study was published in Cell Reports Medicine.
Related topics
Antibodies, Vaccine development
Related conditions
Herpes simplex virus (HSV-1), Herpes simplex virus (HSV-2)
Related organisations
Dartmouth's Geisel School of Medicine, Thayer School of Engineering