Exploring the effects of IFNβ in neuroHIV infection
Posted: 8 April 2024 | Drug Target Review | No comments yet
IFNβ could be developed into a new therapy, following an improved understanding of how innate immunity affects the brain during chronic HIV infection.


Researchers at the University of California, Riverside, have used a mouse model of neuroHIV to investigate the effects of interferon-β (IFNβ), a small protein that is involved in cell signalling and integral to the body’s natural defence mechanism against viral infections. The team discovered that higher or lower than normal levels of IFNβ affect the brain in a sex-dependent manner.
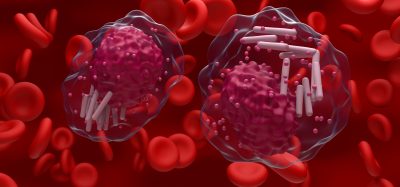
NeuroHIV refers to the effects of HIV infection on the brain or central nervous system (CNS) and, to a lesser extent, the spinal cord and peripheral nervous system. In numerous diseases, including dementia, neuroHIV can cause issues with memory and thinking.
Dr Marcus Kaul, a professor of biomedical sciences in the School of Medicine, led the study. He explained that when infection-induced IFNβ levels become high, the brains of females and males are protected. If infection-induced IFNβ production are absent or too low, HIV can compromise brain function imminently in both females and males. He added: “However, IFNβ also controls other cell and brain functions…If IFNβ is absent, females display reduced nerve cell connections called dendrites in the cerebral cortex, while males show diminished ‘presynaptic terminals,’ another type of nerve cell connection, in the hippocampus.”
Dr Kaul continued: “Paradoxically, in the hippocampus of females and males, the damage to presynaptic terminals by HIV is diminished when IFNβ is absent but the reduction of injury is more pronounced in males.”
This work adds to scientists’ understanding of how innate immunity affects the brain during chronic HIV infection, as, according to Dr Kaul: “Until now, it was not known that normal levels of IFNβ are required for normal memory function and that the absence of IFNβ changes the production of nerve cell components in a sex-dependent fashion.”
Almost all cells in the body can produce IFNβ. IFNβ regulates the production of inflammatory factors in neuroHIV and has two major effects. The first is that it changes the state of a virally infected cell from ‘normal’ to ‘anti-viral,’ making the cells undesirable environments for the virus, even completely shutting down virus production. The second is that IFNβ is released from infected cells as well as specialised cells that, by sensing infected cells, can alert neighbouring cells and the entire body of a viral infection.
“This is how neighbouring cells adapt to become more resistant to viral infection,” Dr Kaul stated. “Some of them will also release additional anti-viral factors and a mixture of other factors that can promote or limit inflammation, such as cytokines called CCL3, CCL4 and CCL5.”
The researchers created a new variant of an established transgenic mouse model of neuroHIV by crossbreeding this model with mice that lacked IFNβ. Then, they analysed memory function and brain tissue of the transgenic mice for injury that typically occurs in neuroHIV. Notably, the mouse model of neuroHIV used shares crucial features of brain injury and compromised function, like impaired memory, with people living with HIV infection, or PLWH.
First author Dr Hina Singh, assistant project scientists in Kaul’s lab, commented: “HIV and some other viruses have developed mechanisms to reduce or even prevent the production of more than normal levels of IFNβ…We know little about the role of IFNβ in the human brain beyond that it can reduce inflammation. This is a major reason why IFNβ is used to treat multiple sclerosis, an autoimmune disease that affects more than 2.8 million people worldwide. Currently, we have almost no information about how much IFNβ is present in the brains of PLWH and what it does there.” She said that the study highlights the importance of having normal levels of IFNβ during no viral infection and having sufficiently high levels of IFNβ in case of neuroHIV or other viral infections.
Moving forward, the researchers aim to confirm the findings of the neuroHIV model in PLWH. Dr Kaul concluded: “Ultimately, we hope to develop IFNβ into a therapy for patients with neuroHIV.”
This study was published in Brain, Behavior, and Immunity.
Related topics
Drug Development, Drug Targets, Protein, Small molecule, Therapeutics, Virology
Related conditions
neuroHIV
Related organisations
University of California Riverside
Related people
Dr Hina Singh (UCR), Dr Marcus Kaul (UCR)