New CAR-T therapy shows promise in leukaemia treatment
Posted: 1 December 2024 | Drug Target Review | No comments yet
Obecabtagene autoleucel (obe-cel) has demonstrated strong efficacy in treating relapsed B-cell leukemia, with high response rates and minimal side effects.
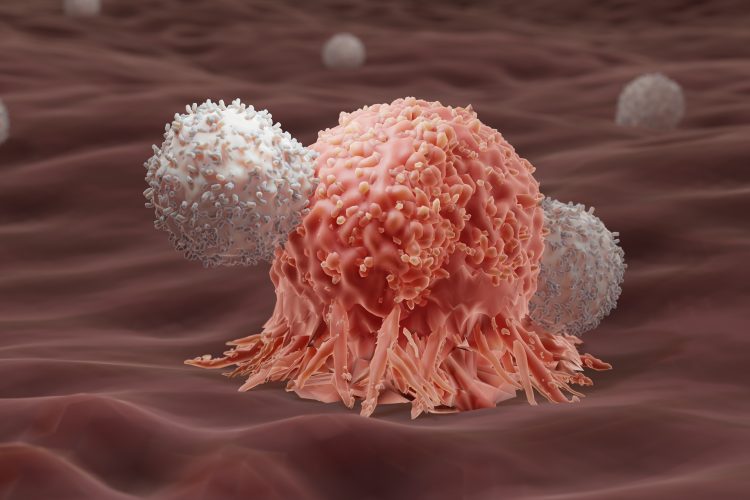
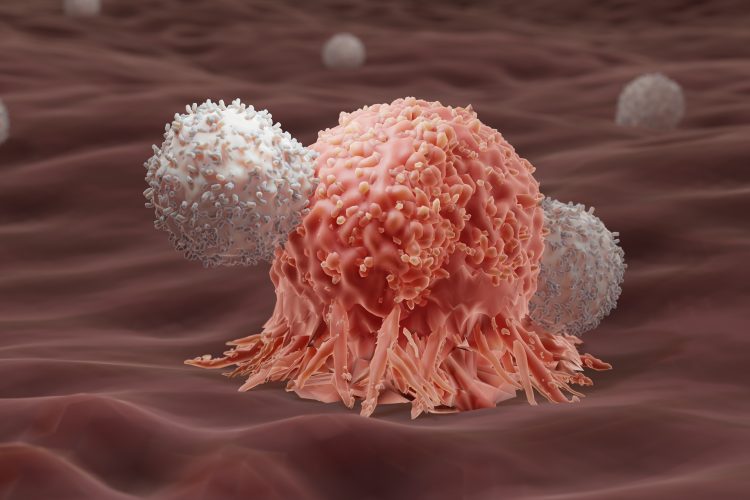
A novel CAR T-cell therapy, obecabtagene autoleucel (obe-cel), has demonstrated strong efficacy in treating patients with relapsed or refractory B-cell acute lymphoblastic leukaemia (ALL). The results from the Phase Ib/II FELIX trial, led by researchers at The University of Texas MD Anderson Cancer Center, showed high response rates and minimal side effects, paving the way for the therapy’s FDA approval in November 2024.
High response rates and survival outcomes
The study, published in the New England Journal of Medicine, reported that 127 evaluable patients with relapsed or refractory CD19-positive B-cell ALL treated with obe-cel had a 76.6 percent response rate and a 55.3 percent complete remission rate. The median overall survival (OS) for infused patients was 15.6 months, with six- and 12-month survival rates of 80.3 percent and 61.1 percent, respectively.
FDA approval marks a milestone for treatment
Based on these promising results, the FDA approved obe-cel for adult patients with relapsed or refractory B-cell ALL. This approval is a significant advancement for this patient population, who previously had limited treatment options. Researchers observed minimal immunotoxicity and a strong persistence of CAR T cells, which supports obe-cel as a potential new standard of care in this area.
“Patients with B-cell ALL need effective standalone treatment options, and obe-cel demonstrated strong long-term efficacy and response rates in patients treated on the FELIX study,” said Dr Elias Jabbour, professor of Leukemia and the study’s U.S. lead investigator.
While some patients did experience side effects associated with CAR T cell therapy, such as cytokine release syndrome (CRS) and neurotoxicity, these effects were generally mild and consistent with previous studies.
Minimal need for stem cell transplantation
Among the 99 patients who responded to obe-cel, only 18 went on to receive a stem cell transplant (SCT) while in remission. This finding suggests that obe-cel provides a durable response that may reduce the need for additional treatments like stem cell transplants.
The trial also highlighted the significant clearance of minimal residual disease (MRD) following obe-cel treatment. MRD refers to a small number of cancer cells that may remain in the body after treatment and potentially cause a relapse. In the study, 68 high-risk patients—those with bone marrow blasts greater than 5 percent prior to lymphodepletion—achieved complete remission, with 58 patients being MRD-negative after obe-cel infusion.
Looking ahead
Dr Jabbour will present further findings from the study at the 2024 American Society of Hematology (ASH) Annual Meeting on December 9, focusing on the correlation between MRD-negative remission depth and clinical outcomes.
This study, funded by Autolus Therapeutics, represents a significant step forward in the treatment of relapsed or refractory B-cell ALL and brings hope for improved outcomes for patients who previously had few options.
This study was published in the New England Journal of Medicine.
Related topics
Biopharmaceuticals, Drug Discovery, Drug Discovery Processes, Immuno-oncology, Immuno-oncology therapeutics, Immunotherapy, Oncology, Therapeutics
Related conditions
B-cell acute lymphoblastic leukaemia (B-ALL), Leukaemia
Related organisations
Autolus Therapeutics, The University of Texas MD Anderson Cancer Center
Related people
Dr Elias Jabbour