In vivo CAR T: Faster, cheaper, and more effective cancer care
Posted: 16 December 2024 | David Fontana (Chief Operating Officer at Umoja Biopharma) | 1 comment
Find out how in vivo cell therapies could transform cancer treatment by providing faster, more affordable, and accessible options for more patients.
Since their first approvals in 2017, autologous CAR T-cell therapies have revolutionised the treatment of blood cancers, offering hope where previous options had failed. However, in their current ex vivo form, a patient’s cells are collected and then modified over weeks or months in a distant manufacturing site. Consequently, these therapies come with significant burdens and are often underutilised despite their transformative patient outcomes.
In this article, David Fontana, Chief Operating Officer of Umoja Biopharma, discusses the organisation’s plans for VivoVec™, its proprietary gene delivery platform. VivoVec™ enables a patient’s body to produce cancer-fighting CAR T-cells in vivo, potentially eliminating the complexity, delays, and high costs associated with current autologous CAR T-cell therapies.
Innovations in CAR T-cell therapy for faster treatment
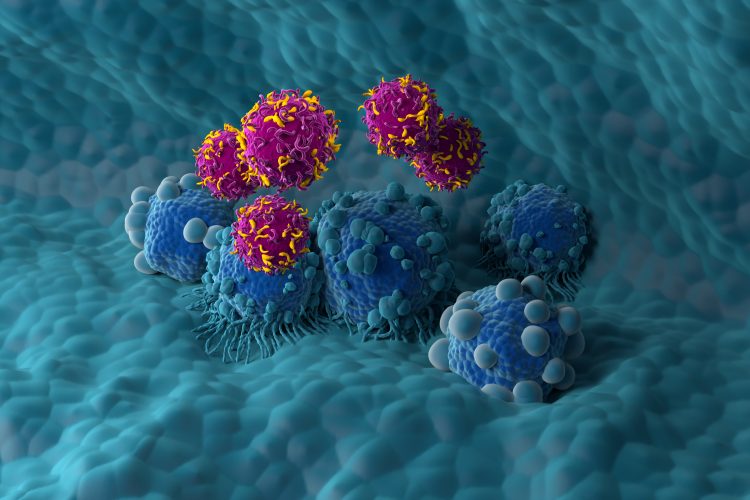
Recent advancements in ex vivo CAR T-cell therapies have revolutionised cancer treatment by harnessing the power of a patient’s own immune system to recognise and fight cancer.
Recent advancements in ex vivo CAR T-cell therapies have revolutionised cancer treatment by harnessing the power of a patient’s own immune system to recognise and fight cancer. Treatment outcomes for large B-cell lymphoma were dismal before CAR T-cell therapies. After two relapses, fewer than 30 percent of patients responded to treatment, and the median overall survival was less than seven months. With the first approvals of CD19 CAR T-cells in 2017, treatment outcomes for patients improved dramatically. Response rates approached 85 percent, with nearly 60 percent of patients achieving a complete response. Median overall survival was extended from seven months to over 25 months in those treated with CAR T cells.
Despite these transformative outcomes, current ex vivo autologous approaches are marked by significant inefficiencies, high costs, and toxicities, all of which limit the widespread use of potentially curative CAR T cells.
As the field of cell and gene therapy continues to evolve, innovative approaches are emerging to overcome these limitations. Today, researchers are exploring new ways to simplify and deliver CAR T cells more quickly, or even generate them directly in the patient’s body, an area of research led by Umoja Biopharma.
Closing the patient access gap with manufacturing
The process of collecting a patient’s cells and shipping them to a manufacturing plant for gene modification is highly manual, limiting the number of treatment sites that can offer these therapies.
Today’s ex vivo CAR T-cell treatment process involves multiple steps that limit treatment availability. The process of collecting a patient’s cells and shipping them to a manufacturing plant for gene modification is highly manual, limiting the number of treatment sites that can offer these therapies. Infrastructure requirements for treatment sites, such as apheresis beds and on-site staff for monitoring, drive high costs, while reimbursement rates are often low. These and other complexities have limited access to CAR T cells to only a small fraction of oncology treatment sites, typically those at large academic teaching hospitals.
For patients, accessing these therapies requires a referral to one of the limited treatment sites, where they must work with a new care team. This process often leads to delays, with waiting periods of up to six weeks to receive their finished CAR T cells. When their drug product is finally ready, they still must undergo multiple days of lymphodepleting chemotherapy along with the added risks of toxicities from pre-treatment.
Each day lost to the burdens of ex vivo CAR T cell treatment represents additional lost time in the critical fight against a patient’s cancer. For patients with aggressive diseases, the waiting time for CAR T-cell treatment may be too long. The denial of even a chance to be considered for treatment represents an efficacy failure of the current ex vivo autologous CAR T class. What good are potentially curative outcomes from CAR T cells if only a subset of eligible patients can navigate the process to receive them?
The promise of in vivo CAR T-cell therapies
Until recently, innovations in this class have been focused on reducing the numbers of days needed to manufacture CAR T cells. Closed and shortened manufacturing systems, as well as using cells from healthy donors, have been explored to reduce the process time by days or weeks.
Umoja’s VivoVec in vivo CAR T-cell generation platform aims to eliminate the treatment and manufacturing gap entirely, transforming what is currently one of the most complex treatment journeys into one more akin to a typical antibody infusion. Effectively, Umoja aims to allow the manufacturing process to occur entirely within the patient’s own body, generating CAR T cells in mere hours instead of months. With this new approach, different companies are exploring various technologies, such as lentiviral and lipid nanoparticles, each offering unique advantages and challenges. Lentiviral platforms offer the potential of a one-time treatment to generate long-lasting CAR T cells in a patient’s body, while other RNA-based platforms offer an approach that uses repeat dosing for short-term generation of CAR T cells.
Published non-human primate data show that Umoja’s VivoVec particles produced CAR T-cells that resulted in a longer, more sustained response in vivo compared to benchmark models using traditional ex vivo processes. The next step is to validate these findings in the clinic.
Umoja’s first clinical trial product, UB-VV111, is a lentiviral drug designed to generate CD19 CAR T-cells directly within a patient’s body, eliminating the need to collect immune cells or administer lymphodepleting chemotherapy beforehand. Following recent IND clearance from the U.S. Food and Drug Administration, Umoja’s Phase 1 clinical trial, INVICTA-1, will be the first in vivo CAR T cell therapy to enter clinical testing in the US. Umoja aims to dose its first patients near the end of 2024 with clinical updates expected in 2025.
Our path to success is further strengthened by our unique investment in controlling our own manufacturing facility. Located in Louisville, Colorado, Umoja’s CLIMB facility accelerates the translation of scientific discoveries into manufactured drug products, while reducing the costs, risks, and extended timelines associated with partnering with contract manufacturers.
The future of in vivo CAR T-cell therapies
In vivo CAR T-cell therapies could represent a transformative step in treatment for those living with cancer and other conditions with high unmet needs, offering the potential to reprogram immune cells directly within the body. However, ongoing research and collaboration are crucial to overcoming remaining barriers and ensuring that more patients can benefit from these groundbreaking therapies.
As clinical trials begin in the coming year, we will have the opportunity to fully realise a future where these treatments are not only more efficient and accessible, but also more effective in delivering life-saving outcomes to all who may benefit.


David Fontana, Chief Operating Officer at Umoja Biopharma
Related topics
Cancer research, Cell Therapy, Clinical Trials, Drug Discovery Processes, Drug Targets, Gene Therapy, Immuno-oncology, Immuno-oncology therapeutics, Immunotherapy, Therapeutics
Related conditions
blood cancers, Cancer, Large B-cell lymphoma
Related organisations
Umoja Biopharma
Related people
David Fontana








An insightful and timely article on the potential of in-vivo CAR-T therapies! It’s exciting to see how advancements in this field could make cancer treatment faster, more affordable, and effective. Looking forward to seeing the future impact of these developments!