Cilta-cel: A new era in multiple myeloma treatment
Posted: 29 January 2025 | Carrie Haslam | No comments yet
New cell therapy, Cilta-cel, shows promise in the treatment of multiple myeloma, providing a personalised approach with the potential for long-term remission.
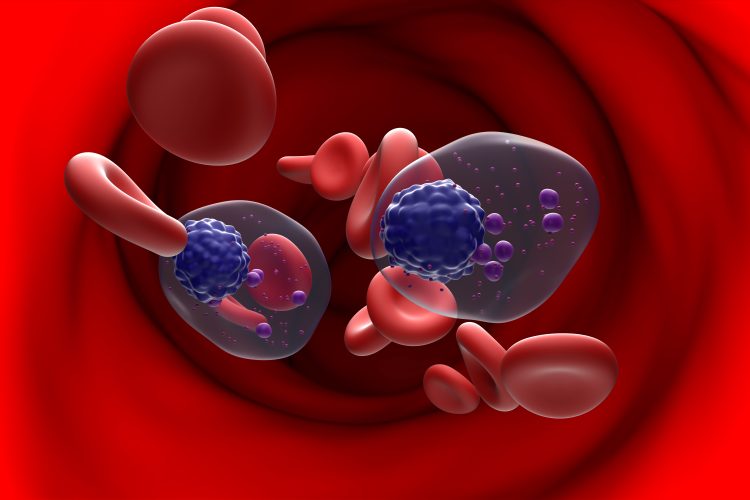
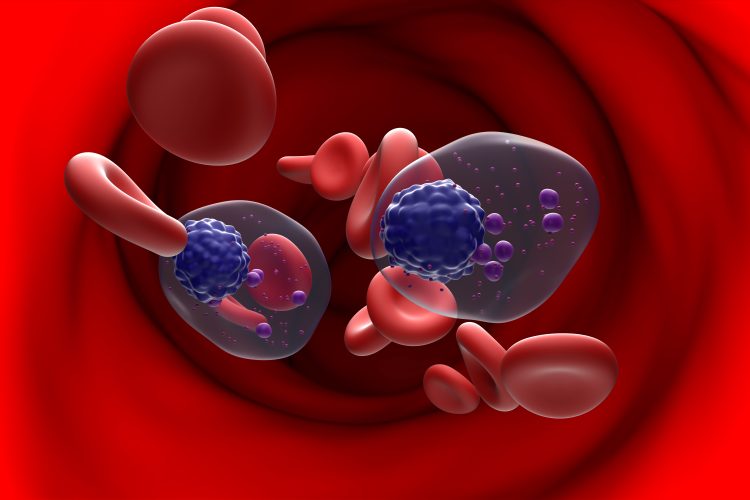
Multiple myeloma is a rare and aggressive blood cancer that originates in plasma cells, a type of white blood cell in the bone marrow. However, in multiple myeloma, the plasma cells become cancerous and produce abnormal antibodies. As these malignant cells accumulate, they crowd out healthy cells in the bone marrow, disrupting the production of vital blood components, such as red blood cells, white blood cells, and platelets. The symptoms of multiple myeloma can be subtle and often mimic those of other conditions, meaning it is typically diagnosed at an advanced stage. Although the disease primarily affects older adults, with the average age of diagnosis being 70, it can also occur in younger individuals. Despite treatment advances, multiple myeloma remains incurable, with many patients experiencing relapses, highlighting the urgent need for more effective long-term therapies.
Recent breakthroughs in treatment are offering renewed hope for multiple myeloma patients, particularly those with relapsed or refractory forms of the disease. Edmond Chan, EMEA Therapeutic Area Lead for Haematology at Johnson & Johnson, recently shared his insights on the promising future of multiple myeloma therapies. With over 12 years of experience in the pharmaceutical industry, Chan discussed how innovative treatments like Ciltacabtagene autoleucel (cilta-cel) are transforming the treatment landscape and significantly enhancing patient outcomes. These advancements not only offer new hope to patients, but they also lay the foundation for a future where multiple myeloma may no longer be a life-limiting disease.
A new era for multiple myeloma treatment
Multiple myeloma is a complex disease, and as Chan highlighted, its treatment has traditionally been challenging, particularly for patients who relapse after initial therapies. “Multiple myeloma has been difficult to manage because of the heterogeneity of the disease and because it often requires multiple lines of therapy.
With cilta-cel, we use the patient’s own T-cells, modify them to enhance their cancer-fighting abilities, and reinfuse them into the body as a one-off infusion.
As patients relapse, the options become limited,” Chan explained. “When patients experience relapse on commonly used drugs like lenalidomide, the disease becomes more difficult to treat.” At this stage, patients are classified as having ‘relapsed and refractory’ multiple myeloma.
This is where cilta-cel, an advanced cell therapy, plays a crucial role. Cilta-cel is a chimeric antigen receptor (CAR) T-cell therapy designed to specifically target B-cell maturation antigen (BCMA) on the surface of malignant plasma cells, making it particularly effective in treating B-cell malignancies like multiple myeloma. By harnessing the power of the patient’s own immune system, cilta-cel targets and eliminates cancer cells. “With cilta-cel, we use the patient’s own T-cells, modify them to enhance their cancer-fighting abilities, and reinfuse them into the body as a one-off infusion,” Chan explained. This innovative technique has delivered remarkable results for patients who previously had limited treatment options.
Achieving MRD negativity
A key breakthrough with cilta-cel is its ability to induce MRD (Minimal Residual Disease) negativity. MRD negativity means the absence of detectable cancer cells, even at the most sensitive levels of detection. “In our trial, we were able to achieve MRD negativity at the 10^-5 level, meaning that no cancer activity was detectable,” Chan highlighted. “MRD negativity is associated with long-term survival and sustained remission.” This is a significant achievement and a major milestone in the treatment of multiple myeloma.
When patients experience relapse on commonly used drugs like lenalidomide, the disease becomes more difficult to treat.
For patients with relapsed multiple myeloma, these results could be transformative. The study revealed that patients who achieved sustained MRD negativity were five times more likely to remain free of disease activity for over 12 months. “This is a huge step forward because for the first time, we have a treatment that works effectively for a patient population that has had very few options,” says Chan.
Long-term impact
In addition to the promising initial results, long-term data from cilta-cel has demonstrated significant benefits. Chan noted that after nearly three years of follow-up, patients who received cilta-cel showed improved progression-free survival (PFS) and overall survival (OS). “Multiple myeloma tends to relapse over time, but cilta-cel is showing not only faster responses but also longer periods without relapse,” Chan explained. This long-term benefit is crucial for patients who would otherwise face cycles of relapse and retreatment. For patients, this translates to the potential for a longer and better quality of life. “In patients who are difficult to treat, we now have a chance to provide them with a better quality of life and extended survival,” he added.
In patients who are difficult to treat, we now have a chance to provide them with a better quality of life and extended survival.
One of the key innovations of cilta-cel lies in its personalised treatment approach. This therapy enables the development of individualised treatment plans tailored to each patient’s unique needs. For patients whose multiple myeloma no longer responds to first-line therapies, cilta-cel provides an alternative that could offer the potential for long-term remission. This personalised strategy marks a significant departure from the traditional one-size-fits-all approach in cancer treatment, especially in the context of hematologic cancers.
Who is affected and how new treatments can help
Multiple myeloma predominantly affects older adults, and for these patients, the potential benefits of cilta-cel are especially profound. Chan explained that for elderly patients who are not candidates for aggressive or ongoing treatments, cilta-cel can offer the possibility of living without disease activity for extended periods. “For many elderly patients, cilta-cel could be the only treatment they need,” allowing them to live their later years without the burden of constant cancer therapy.
Early intervention
Looking ahead, Chan is excited about the potential for using cilta-cel earlier in treatment, possibly even before the disease relapses. “We are also studying cilta-cel in earlier lines of therapy, not just for relapsed patients, but for newly diagnosed multiple myeloma patients,” he explained. Clinical trials, such as CARTITUDE-5 and CARTITUDE-6, are investigating the benefits of cilta-cel as a front-line therapy.
This approach has the potential to revolutionise the management of multiple myeloma. Rather than waiting for the disease to relapse, cilta-cel could be used earlier to improve outcomes and possibly even cure patients. While Chan emphasised that this remains a long-term goal, the opportunity to fundamentally change treatment strategies is an exciting prospect for both clinicians and patients.
Johnson & Johnson’s commitment to innovation
Chan concluded by emphasising Johnson & Johnson’s commitment to advancing treatments for hematologic cancers and the important work being done in the company’s haematology division. “We are pushing the boundaries of science to develop treatments that not only extend life but also improve the quality of life for patients,” he said. He also emphasised the crucial role of collaboration with healthcare providers and patients in driving innovation, highlighting how these partnerships are essential to advancing new treatments. “We can’t achieve breakthroughs without the support of the scientific community, patients and their families,” Chan explained.
Therapies like cilta-cel offer a promising future for multiple myeloma treatment. These innovations not only hold the potential for longer survival but also for better quality of life for patients who have had limited options in the past. As new data emerges, there is growing hope that these treatments could eventually lead to a cure, transforming the lives of patients worldwide. With leaders like Edmond Chan driving progress, the fight against multiple myeloma is just beginning, and the future of cancer treatment looks brighter than ever.
Meet Dr Edmond Chan


Dr Edmond Chan has been with Johnson & Johnson (J&J) for just over twelve years, where he is currently the head of the EMEA Medical Affairs Haematology team, focusing on haematological cancers and driving patient centred solutions and treatment in areas of unmet medical need. He started at J&J in R&D before moving into medical affairs; working in the areas of diabetes and immunology before settling into haemato-oncology. Edmond has also worked as an ABPI final signatory and holds a PhD in Medical Research in Therapeutic Antibodies as well as a Master’s in Medical Statistics from the London School of Hygiene and Tropical Medicine. He is an experienced, UK-trained pharmaceutical physician specialising in renal medicine with over 12 years’ experience in clinical practice.
Related topics
Antibodies, Antibody Discovery, Cell Therapy, Chimeric Antigen Receptors (CARs), Immuno-oncology, Immuno-oncology therapeutics, Personalised Medicine, Precision Medicine, T cells, Therapeutics
Related conditions
multiple myeloma
Related organisations
Johnson & Johnson
Related people
Edmond Chan