Experts explore the future of iPSC-based cell therapies
Posted: 19 February 2025 | | No comments yet
Discover the transformative potential of iPSC-based therapies in regenerative medicine, alongside their challenges including scalability, safety and targeted delivery.
Regenerative medicine is set to be transformed by induced pluripotent stem cells (iPSCs). These versatile cells can be reprogrammed to become virtually any cell type in the human body, offering groundbreaking possibilities for treating a wide range of conditions, from genetic disorders to degenerative diseases. Their capacity to provide an unlimited supply of cells means that iPSCs could revolutionise cell therapies.
Unlike embryonic stem cells, iPSCs avoid the ethical dilemmas tied to embryo use, broadening access to innovative therapeutic applications. However, despite their promise, iPSCs face significant challenges that must be addressed before they can fully realise their potential as a cornerstone of regenerative medicine.
These challenges were the focus of a panel discussion at the 2024 Advanced Therapies Europe (ATE24) conference, led by two prominent experts: Dr Boris Greber, Head of R&D, iPSC at Catalent Cell & Gene Therapy in Europe, and Dr Frederic Cedrone, Vice President of Corporate Innovation at Catalent. Together, they shared valuable insights into the progress of iPSC-based therapies, the key obstacles ahead and the exciting opportunities for future breakthroughs.
The promise of iPSCs
The discussion began by highlighting the key advantages of iPSCs, with one of the most notable being their capacity to serve as an unlimited source of material. Unlike adult stem cells, which are often limited in availability and challenging to harvest from patients, iPSCs can be derived from any somatic cell – such as skin or blood – and reprogrammed into pluripotent cells. This ability to create a renewable, scalable supply of cells positions iPSCs as a highly promising tool for advancing regenerative medicine.
The ethical benefits of iPSCs were also emphasised, with experts noting their increasing significance to both biopharmaceutical companies and investors. As the industry continues to embrace iPSCs as a cornerstone for developing regenerative therapies, these ethical advantages have become a key driver of innovation and investment. In addition, iPSCs enable allogeneic therapies, where treatments can be developed without the need to match donor and recipient cells. This breakthrough overcomes the immunological rejection challenges typically associated with stem cell transplants, broadening the pool of eligible patients and simplifying the treatment process.
Despite these promising advantages, there are several significant hurdles to overcome before iPSCs can be fully integrated into clinical practice. Both Cedrone and Greber discussed the critical challenges surrounding the large-scale manufacture of iPSCs while ensuring their quality and genomic stability. The remarkable capacity of iPSCs to self-renew and differentiate into any cell type makes them a highly versatile tool, but it also means they can accumulate mutations over time, particularly when expanded over extended periods. This introduces the risk of tumourigenesis, where mutations could lead to uncontrolled cell growth and potentially result in cancer. To mitigate this risk, rigorous monitoring and quality control measures are essential.
Greber, who leads the iPSC R&D efforts at Catalent, highlighted the importance of maintaining genomic stability:
“With regards to genomic integrity, given their unlimited expansion capability, iPSC generation and expansion through multiple population doublings certainly bears risk for new, potentially cancer-causing mutations, in addition to those in the founder cell,” Greber explained.
iPSC generation and expansion through multiple population doublings certainly bears risk for new, potentially cancer-causing mutations, in addition to those in the founder cell.
“At Catalent, our lines are derived from clinical-grade cord blood units, which we consider a safety measure. For example, we have shown that these neonatal starting cells indeed have a lower mutation load as compared to adult ones and that this translates into the iPSCs, resulting in a reduced mutational burden. Moreover, as said in our QC panel, we use whole genome sequencing and other assays to further assess genomic integrity and mutations in cancer-related genes at the iPSC banking stage in a stringent manner.”
Balancing quantity and quality in iPSC manufacturing
Another major challenge highlighted by both panellists was the scalability of iPSC production. While iPSCs hold enormous therapeutic potential, producing a sufficient quantity of high-quality cells for widespread clinical use remains a hurdle. The need to generate billions of cells for therapies – while ensuring the quality and consistency of the original iPSC line – is no easy task. Cedrone discussed the ongoing efforts to scale iPSC production, citing a few innovative approaches that have shown promising results.
“Today we see several scaling approaches being developed,” he explained. “Two promising examples include specialised suspension bioreactors (with or without microcarrier technology), or 3D suspension with technology pioneered by a few innovators in the field, such as TreeFrog Therapeutics, which involves growing iPSCs in an alginate-based capsule (C-StemTM platform- Link).”
While these technologies are encouraging, Cedrone stressed that the challenge is not solely about producing more cells, but also ensuring that the cells retain their ability to differentiate into the desired cell types.
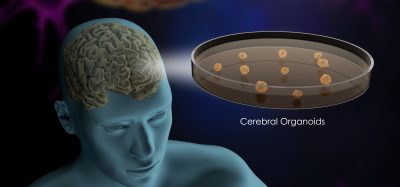
“The question here is more on the delivery device or system – we are missing delivery systems that can deliver billions of cells to the right place and ensure they stay there. This can include tricky areas such as the brain, pancreas and liver. For example, maintaining cardiomyocytes in place in the heart is a challenge,” Cedrone revealed. “For instance, an injected single-cell suspension may easily escape the site of injection in that continuously moving organ. However we do see companies innovating in this area and some key developments are emerging, like matrices or injection catheters.”
Regulatory standards: an enabler for iPSC advancement
In addition to scalability, both Cedrone and Greber addressed the challenges of ensuring the safety and stability of iPSCs throughout the development process. Regulatory requirements play a crucial role in this, as the approval of iPSC-based therapies will depend heavily on meeting high safety and quality standards. As Greber pointed out, addressing regulatory concerns early in the development process is essential.
At Catalent we have developed our processes and cell lines with regulatory guidelines in mind from the beginning.
“At Catalent we have developed our processes and cell lines with regulatory guidelines in mind from the beginning. In some cases, we also had to look ahead and anticipate future directions. For example, early on, we implemented whole genome sequencing at >50x coverage to assess mutation load in our GMP iPSC lines. Earlier this year, it was then rewarding to see that regulatory agencies are planning to make this a future requirement.”
Cedrone echoed this perspective, emphasising that regulatory guidelines should be viewed as an enabler, not a barrier.
“Contrary to popular opinion, regulation is not a hurdle, but rather an enabler. If the data package (including safety) is well thought out and developed from the beginning, regulations can be a support to frame the development journey. The difficult area right now is around scale – ie, manufacturing dozens of billions of cells and differentiating these at scale while maintaining the quality of the starting material (the iPSC line) and the final product. This is not a trivial task!”
In conclusion, while the potential for iPSC-based therapies is vast, there are significant hurdles to overcome before these therapies can be widely adopted. Ensuring scalability, safety and targeted delivery of iPSCs will require continuous innovation and collaboration across the industry. However, with the expertise and dedication of leaders like Fred Cedrone and Boris Greber, the future of iPSC-based regenerative medicine looks incredibly promising. The journey towards successful iPSC-based therapies will not be without its challenges, but careful planning and concerted efforts will surely bring these transformative therapies to the patients who need them most.
Featured experts:




Dr Frederic Cedrone is the Vice President of Corporate Innovation at Catalent, where he works closely with the Cell and Gene Therapy teams to drive innovation in emerging therapeutic modalities through strategic partnerships, licensing and technology acquisitions. Cedrone joined Catalent in 2022, bringing with him 18 years of experience in biotech, including key roles at Lysogene SA and Cellectis SA. His areas of expertise include biologic drug development, cell and gene therapies, and gene editing. Cedrone holds a PhD in molecular biology and enzyme engineering from Marseille University, France.
Related topics
Cell Therapy, Gene Therapy, Induced Pluripotent Stem Cells (iPSCs), Regenerative Medicine, Stem Cells
Related organisations
Catalent
Related people
Dr Boris Greber, Dr Frederic Cedrone