Specialised blood vessels enhance tumour-fighting immunotherapy
Posted: 19 April 2017 | Niamh Marriott (Drug Target Review) | No comments yet
The successful combination of two therapies results in the growth of specialised vessels that deliver cancer-fighting immune cells to a tumour, potentially leading to more effective treatments and longer survival periods.
Scientists from VIB and KU Leuven, together with colleagues from the University of California and the Swiss Institute for Experimental Cancer Research have demonstrated that anti-angiogenic therapy can improve immune boosting treatments.
Sustained angiogenesis, the growth of new blood vessels, and the suppression of the immune system are hallmarks of cancer, with an increasing amount of evidence demonstrating that these two activities are interrelated. Therapies that prevent tumour blood vessel growth are often used in clinics to fight cancer – but they are only effective in a particular subset of patients.
Similarly, the recent successes to directly stimulate the immune system with inhibitors of negative immune checkpoint regulators – such as antibodies against programmed cell death protein 1 (PD-1) or its ligand PD-1 – has led to many clinical trials. However, only a minority of treated patients have responded to these immunotherapies, emphasising the need to identify strategies that will increase response rates in patients.
Dr Elizabeth Allen and colleagues provide evidence that anti-PD-L1 therapy can sensitise and prolong efficacy of anti-angiogenic therapy, and conversely, anti-angiogenic therapy can improve anti-PD-L1 treatment specifically when intra-tumoural HEVs are generated that facilitate enhanced cell infiltration, activity and tumour cell destruction.
Blood vessels help regulate immunity
To avoid being targeted by their hosts’ immune systems, tumours maintain an immunosuppressive environment by manipulating the characteristics of the immune and vascular system. Increased blood supply and decreased immune activity are necessary for malignant cells to multiply.
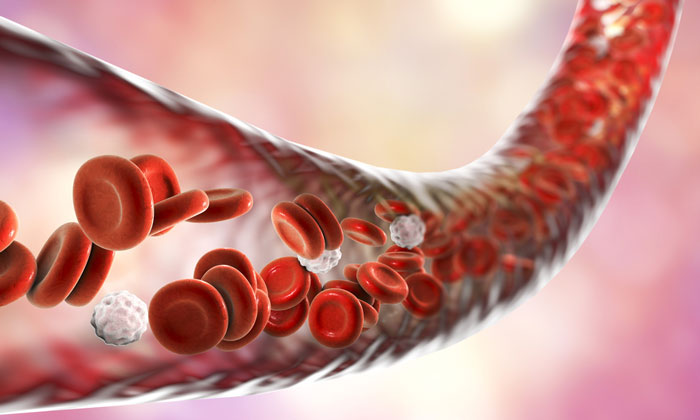
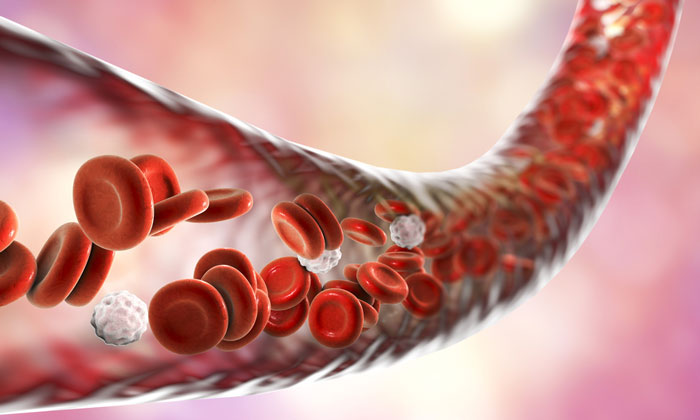
Prof Dr Gabriele Bergers (VIB-KU Leuven): “The network of blood vessels itself is an important regulator of immunity because it controls white blood cell traffic. By preventing the infiltration of white blood cells, the cancer is able to evade the host’s immune system.”
A counter-intuitive outcome
Interestingly, the team showed that combining anti-angiogenic and immune-stimulating therapies in the treatment of tumours in mouse models resulted in better therapeutic outcomes by providing white blood cell gates through which they can infiltrate cancers.
Dr Elizabeth Allen (VIB-KU Leuven): “It was interesting to observe that this combination of immune system-activating and anti-angiogenic antibodies causes a positive feedback loop. The result is the growth of specific blood vessels that deliver cancer-fighting immune cells into the tumour. These high endothelial venules (HEVs) are normally found in lymphoid organs such as lymph nodes, where they help transport white blood cells. For the first time, we showed that the growth of HEVs can be therapeutically induced in tumours.”
Describing the process
The results of the study indicate that the two therapies stimulated significant growth of HEVs in pancreatic and mammary tumours, leading to malignant cell death and tumour shrinkage. The next step in this research involves investigating how intra-tumoural HEVs are formed and maintained.
Prof Gabriele Bergers (VIB-KU Leuven), “Understanding the underlying mechanisms of the process will contribute to the overarching goal of developing new therapeutic approaches to boosting the immune system in tumours.”
Related topics
Immuno-oncology, Immunology, Immunotherapy
Related organisations
California University, Flanders Interuniversity Institute for Biotechnology (VIB), KU Leuven, Swiss Institute for Experimental Cancer Research
Related people
Dr Elizabeth Allen, Prof Dr Gabriele Bergers