Improving the safety of CRISPR for the clinic
Posted: 9 December 2021 | Dr Danilo Maddalo (Genentech) | No comments yet
Dr Danilo Maddalo from Genentech outlines the main benefits of CRISPR within the clinical realm and highlights some of the safety concerns that must be considered before CRISPR products reach patients.
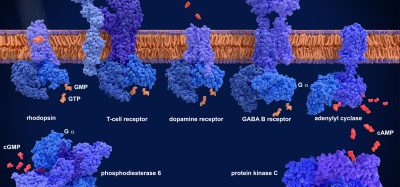
CRISPR technology has huge potential for clinical applications. It can be applied to precisely engineer cells ex vivo that can then be re-infused back into the patient, for example T cells. CRISPR can also be used to correct genes in vivo, an application that would change the way rare genetic diseases are treated and managed. Last but not least, the technology can be applied in the field of diagnostics, another very promising avenue.
However, when a new technology develops so quickly and has so much potential, it is almost natural to have concerns about its safety. Even if scientists have demonstrated that CRISPR is relatively precise – when the correct single guide RNA (sgRNA) is designed – it is still comparable to handling a very sharp knife that can leave unintended cuts around the genome.
A case-by-case approach should always be used when validating the safety of products involving CRISPR. First to consider is which genome editing tool is employed (Cas9, nickase, base editors), as each tool will have unique safety concerns. Moreover, a more careful approach will be needed if more than one sgRNA is used. Lastly, the type of cell to be edited will play an important role, as we know that the DNA repair machinery can vary. As a more general rule, a sequencing strategy to detect unintended genetic modifications such as mutations, indels and chromosomal rearrangements should always be included. Also, these findings should be correlated with in vitro and/or in vivo assessments of cell transformations in the mid-term.
CRISPR technology has huge potential for clinical applications”
In a new study,1 two assays, soft agar colony forming (SACF) and growth in low attachment (GILA), were used to evaluate the transforming potential of a CRISPR-Cas9 system. It was shown that these in vitro assays could predict the cell transformation better than a standard in vivo growth assay, which therefore represents a more time consuming and less cost-efficient approach. The study clearly showed that both SACF and GILA are reliable assays that can be added to the safety assessment package when developing CRISPR-related therapies.
As with any research project, there were many challenges, especially when it came to comparing two approaches (in this case in vitro and in vivo transformation assays). Perseverance and hard work, however, drove this project through the most difficult moments, mostly because of the great team of people working on it.
Article: CRISPR-Cas9-based gene dropout screens: a powerful platform for drug discovery
I believe that in the future, more pre-clinical studies will use a similar method to determine the safety of CRISPR products before they reach the clinic, even if it will also depend on the type of genome editor used. In general, the assays are robust, cheap and quick; they are also a great addition to the pre-clinical package to assess the safety of CRISPR therapies.
Thinking more broadly about the industry, with the constant evolution of the CRISPR toolbox, more assays will be needed to build up a reliable safety package.
About the author
Dr Danilo Maddalo completed his PhD at the Karlsruhe Institute of Technology in Germany and specialised in genome editing and oncology at the Memorial Sloan Kettering Cancer Center, US, before opening a lab at the Novartis Institute for Biomedical Research in Switzerland. He is currently a Senior Scientist at Genentech in San Francisco where he leverages genome editing tools to generate in vivo models of disease to address scientific questions related to oncology and drug discovery.
Reference
- Lemmens M, Fischer B, Zogg M, Rodrigues L, Kerr G, et al. Evaluation of two in vitro assays for tumorigenicity assessment of CRISPR-Cas9 genome-edited cells. Molecular Therapy – Methods & Clinical Development. 2021;23:241-253.