HPV-associated head and neck cancers identified
Posted: 21 August 2023 | Taylor Mixides (Drug Target Review) | No comments yet
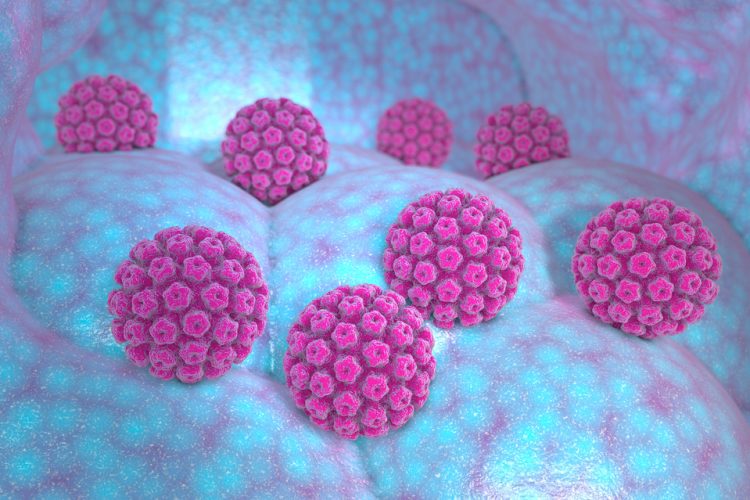
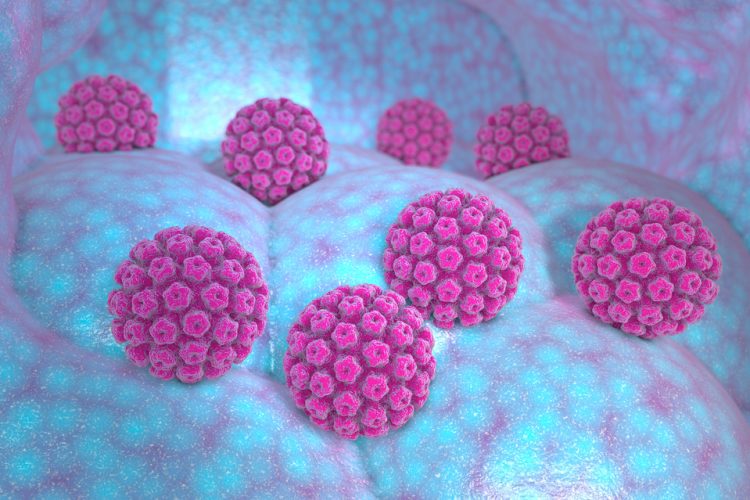
Human papillomavirus (HPV)-associated head and neck cancers, specifically head and neck squamous cell carcinoma (HNSCC), are on the rise worldwide. Yet, the factors contributing to these tumours and their varying responses to treatment remain poorly understood.
To unravel the mysteries behind the treatment response, researchers from the Department of Otolaryngology/Head and Neck Surgery at UNC School of Medicine collaborated with experts from Yale Cancer Center, the Yale Head and Neck Cancer Specialised Program of Research Excellence (SPORE), and the ECOG-ACRIN Cancer Research Group.
Their study, published in Proceedings of the National Academy of Sciences, unveiled the existence of two distinct subtypes of HPV+ head and neck cancers. These subtypes play a pivotal role in determining how patients respond to therapy, with one subtype exhibiting greater responsiveness to radiation therapy. Furthermore, the research revealed a new mechanism of HPV carcinogenesis, which advances efforts towards personalised treatment for patients diagnosed with HPV+ HNSCC.
“We’re the first ones to describe these two subtypes,” explained Wendell Yarbrough, MD, MMHC, FACS, the Thomas J. Dark Distinguished Professor of Otolaryngology/Head and Neck Surgery, “Using this research, we can firmly identify two groups of patients and are able to associate their tumour subtype with treatment outcomes.”
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
Currently, many patients with HPV+ HNSCC receive high doses of radiation combined with chemotherapy, which can result in long-lasting side effects such as muscle fibrosis, swallowing difficulties, and artery hardening. Personalised therapy could enable oncologists to make more informed treatment choices for their patients. However, determining the type and intensity of treatment is challenging without knowledge of the tumour’s response to therapy.
To address this challenge, Yarbrough’s team, including co-authors Travis Schrank, MD, PhD, Natalia Isaeva, PhD, and Wesley Stepp, MD, PhD, coordinated a research cohort at UNC and gathered publicly available data from the University of Chicago and validation data from E1308, a large national cooperative group clinical trial conducted through ECOG-ACRIN.
Through meticulous analysis of tumour samples, the researchers identified several groups of co-expressed genes, with one set standing out for distinguishing tumours with high and low expression. Genes in this set represented targets of a master transcription factor called NF-kB, which plays crucial roles in inflammation, cell death, and the carcinogenesis of HNSCC.
Surprisingly, the two distinct subtypes identified were directly linked to patient outcomes. Tumours with low NF-kB activity were associated with a worse prognosis, whereas tumours with high NF-kB activity were linked to a better prognosis.
These subtypes exhibited remarkable differences in mutated genes, factors driving mutations, number of mutations per cancer, HPV gene expression, HPV integration, gene methylation, and infiltration of specific immune cells into the tumour.
Stepp, a co-author on the paper, played a crucial role in organising the patient set from the UNC cohort, while the collaborative efforts of all organizations involved were instrumental in the success of this research project.
“Tumours with high NF-kB activity were more responsive to radiation therapy, potentially contributing to improved patient survival,”
Notably, patient survival was the most significant distinction between the two tumour subtypes. To gain further insights into the better outcomes observed in one subtype, the researchers created cellular models of each subtype in the laboratory.
“Tumours with high NF-kB activity were more responsive to radiation therapy, potentially contributing to improved patient survival,” Yarbrough explained. “We know that there’s something about activating the NF-kB pathway that makes the tumours more sensitive to radiation therapy, which could explain how and why those patients are surviving better.”
Ultimately, this data could be harnessed to identify patients who may safely undergo de-intensified therapy, reducing side effects and improving their quality of life. With a better understanding of the new mechanism of HPV carcinogenesis, these findings may pave the way for the development of new, personalized treatments that are more effective and have fewer side effects.
Related topics
Gene Therapy, Immuno-oncology, Personalised Medicine, Targets
Related organisations
ECOG-ACRIN Cancer Research Group., Yale Cancer Center, Yarbrough