Targeting CD40 with bispecifics to outsmart tumours
Posted: 11 November 2024 | Søren Bregenholt (Alligator Biosciences) | No comments yet
Søren Bregenholt, Chief Executive Officer at Alligator Bioscience, elucidates how creating bispecific antibodies that target both tumour-specific antigens and CD40, a receptor on the immune system’s dendritic cells, is a new approach that aims to trick tumours into telling the immune system how best to attack.
Immunotherapy has emerged as a powerful tool in our fight against cancer. By mobilising the body’s immune system, this approach offers new hope for patients.
However, despite impressive advancements, many patients still do not respond to current immunotherapy treatments. This is partly because cancer cells are shrewd and often develop ways to evade immune detection. To overcome these escape mechanisms researchers are exploring a wider arsenal of therapeutic strategies.
An important puzzle to solve is how to mount a good immune response in types of cancer with poor T-cell infiltration, or deficiencies in T-cell priming, and associated unresponsiveness to established immunotherapies. These types of cancer represent a significant unmet medical need in oncology.
Harnessing CD40
One potential mechanism is stimulating CD40, a master switch on dendritic cells to activate and orchestrate T cell-mediated immune responses. Prior attempts to target CD40 have been limited to varying degrees by unwanted immune activation causing side effects. Recently, mitazalimab, Alligator Bioscience’s stimulatory monospecific CD40 antibody, has demonstrated success as a potential first-line treatment for pancreatic cancer. Data recently published in The Lancet Oncology showed a substantial overall survival benefit and unprecedented duration of response.1
This mechanism is now being advanced to the next level with CD40 bispecific antibodies carrying tumour-targeting binding parts, which have several advantages and are expected to provide both improved safety and anti-tumour efficacy.
Specific targeting
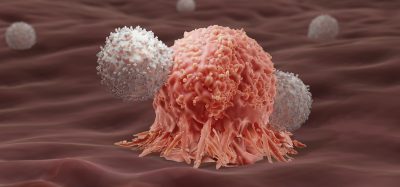
The mechanism delivers a strong immune activation localised to the tumour area, rather than an unwanted systemic activation, thus minimising the possibility of side effects and increasing safety. Tumour targeting also increases anti-tumour efficacy and boosts anti-tumour T-cell response compared to monospecific CD40 agonists. The supposition for this is that the bispecific CD40 antibodies can capture material from cancer cells and physically deliver them to the immune system, enabling higher activation of neoantigen-specific T cells with a very powerful anti-tumour effect.
The presence of a highly expressed tumour antigen, acting as a second target molecule to partner with CD40, is vital as it enables these antibodies to capture tumour parts, or exosomes, and deliver them to dendritic cells. The tumour material contains mutated tumour proteins, called neo-antigens, which are unique to each tumour and are the material that makes the tumour vulnerable to immune attacks. In this way, the tumour can be tricked into telling the immune system how best to effectively attack the tumour cells.
This progress has been facilitated using internal technologies to isolate binders with desired properties and engineer functional and developable bispecific antibody molecules.
The isolation of binders that possess the specific required properties is possible via reference to two so-called antibody libraries. Each of these are proprietary collections of 10^10 different antibody binders, with distinct specific sequences in the six so-called hypervariable regions that constitute the antibody surface that binds to the target molecules. Common for all binders are scaffold regions of human origin that are particularly well suited for the generation of therapeutic antibodies.
With methodologies like phage display and high-throughput screening that leverage next-generation sequencing and advanced data analytics, it is now possible to isolate unique binders with tailored binding and function to a given target, as well as near-perfected developability and manufacturability properties.
The next step for generating bispecific candidate drugs is to combine the isolated binders into a bispecific molecule using a so-called bispecific antibody format, prominent for its geometry and inherent stability, which enable the generation of bispecific antibodies with bivalent interaction to each target and drug-worthy properties.
Preclinical data, published in Journal for ImmunoTherapy of Cancer, have shown how antibodies produced in this manner induced clustering of tumour debris and CD40-expressing cells in a dose-dependent manner. The data demonstrated superior T-cell priming when added to dendritic cells, antigen-containing tumour debris or exosomes, and that the antibodies induced tumour-associated antigen-conditional CD40 activation both in vitro and in vivo, which shows the potential for a wide therapeutic window.2
The first product candidate generated using this approach is a bispecific CD40 agonist, known as ATOR-4066, which has shown significant potential in preclinical development. This has been highlighted in poster presentations at the American Association for Cancer Research (AACR) and the Society for Immunotherapy of Cancer (SITC).
The AACR presentation showed that ATOR-4066 activates tumour-infiltrating dendritic cells and macrophages, resulting in increases in activated tumour-infiltrating T cells. It thus creates a pro-inflammatory tumour microenvironment leading to single-agent complete responses in translational tumour models. It also has potential to induce strong anti-tumour responses in CEACAM5-expressing tumours. CEACAM5 is a tumour-associated antigen that is highly expressed in many cancers, making it an ideal target.3
The second presentation at SITC further underlined the superior anti-tumour effect compared to CD40 monospecific antibodies and detailed an enhanced effect when combined with anti-PD-1 – emphasising potential both as a monotherapy and in combination with checkpoint inhibitors. The data showed activation of CD40-expressing cells was CEACAM5-conditional with no activation in the absence of CEACAM5, indicating a potential for a wide therapeutic window. ATOR-4066 was also shown to induce immunological memory in vivo and capable of clearing homologous tumours upon re-challenge.4
The concept of bispecific antibodies, targeting the validated CD40 receptor and harnessing the power of the immune system, can create an immunological response that will be effective against the tumour’s vulnerabilities, even if the tumour mutates. The aim is to activate immunological cascades that counterbalance potential T-cell deficiencies in many indications and attack tumours from multiple angles, leaving them with nowhere to hide.
The hope, supported by the evidence generated so far, is that this approach will eventually provide a significant improvement in treatment options – particularly in difficult-to-treat indications, such as colon, gastric and lung cancers.
References
1 Borbath I, Geboes P, Laethem J-L, et al. Combining CD40 agonist mitazalimab with mFOLFIRINOX in previously untreated metastatic pancreatic ductal adenocarcinoma (OPTIMIZE-1): a single-arm, multicentre phase 1b/2 study. The Lancet Oncology. 2024: 25(7):853-864. Available from: https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(24)00263-8/abstract
2 Ellmark P, Deronic A, Hagerbrand K, et al. Bispecific antibodies targeting CD40 and tumor-associated antigens promote cross-priming of T cells resulting in an antitumor response superior to monospecific antibodies. 2022: 10. Available from: https://jitc.bmj.com/content/10/11/e005018
3 Andersson H, Celander M, Ellmark P, et al. Abstract 5309: ATOR-4066, a Neo-X-Prime™ bispecific antibody targeting CD40 and CEACAM5, induces tumor localized immune cell activation in preclinical in vivo tumor model. 2024: 84(6). Available from: https://aacrjournals.org/cancerres/article/84/6_Supplement/5309/739403/Abstract-5309-ATOR-4066-a-Neo-X-PrimeT-bispecific
4 Andersson H, Celander M, Ellmark P, et al. 837 Combination treatment with ATOR-4066, a Neo-X-Prime™ bispecific antibody targeting CD40 and CEACAM5, and anti-PD-1 reverses T cell exhaustion in vitro. 2023: 11(1). Available from: https://jitc.bmj.com/content/11/Suppl_1/A935
About the author
Søren Bregenholt, Chief Executive Officer of Alligator Biosciences


Related topics
Antibodies, Drug Development, Immuno-oncology
Related conditions
Cancer
Related organisations
Alligator Biosciences
Related people
Søren Bregenholt (Alligator Biosciences)