Alzheimer’s disease: driving advancements with precision medicine
Posted: 25 October 2024 | Simon Lovestone (Johnson & Johnson) | No comments yet
In this Q&A, Simon Lovestone, Vice President, Global Head, Neuroscience Discovery and Translational Science at Johnson & Johnson, shares how they are leveraging the A/T/N biomarker framework to achieve breakthroughs in Alzheimer’s disease research, in an aim to alter disease progression before daily life is significantly affected.
How does precision neuroscience differ from traditional approaches in the treatment of neurodegenerative diseases, and what advantages does it offer?
Traditionally, Alzheimer’s disease is diagnosed by clinical examination, medical history and cognitive testing.1 While these approaches have been the basis of Alzheimer’s disease diagnosis for many decades, they are based on evaluating clinical symptoms, not disease pathology. Many of the clinical symptoms of Alzheimer’s disease, like memory loss, overlap with symptoms associated with normal ageing and other neurodegenerative disorders, creating a need for precision during the diagnosis process.2
In the future, we hope to be able to recognise and diagnose Alzheimer’s disease much earlier. At Johnson & Johnson, our differentiated Alzheimer’s disease research program is focused on leveraging the latest advancements in precision medicine, data science and digital health to help make earlier diagnosis an option and help treat the right patient with the right treatment at the right time.
More specifically, our research teams are focused on the tau protein and studying digital, blood and imaging biomarkers to aid development programs and decision making within them. We’re investigating powerful tools that may allow for an earlier – and biologically based – prediction of Alzheimer’s disease, which are being evaluated to help identify patients for clinical trials. We hope to leverage these advancements and technologies to monitor disease progression and measure the therapeutic effect in our development programs.
Can you elaborate on the significance of the “A/T/N” biomarker framework for Alzheimer’s disease and how it has advanced our understanding of the disease’s pathophysiology?
We believe we are at a breakthrough moment in Alzheimer’s disease research. As a company that has been in this space for decades, we’ve been able to learn from our successes, our past experiences and evolving scientific advancements over time to shape the strategy we have in place today: to alter the course of the disease well before daily function is affected. Biomarkers are an essential advancement that will help determine risk for developing Alzheimer’s disease, diagnose the disease before symptoms have progressed significantly, predict how quickly patients may experience cognitive decline and evaluate how well new therapies are working.1,3
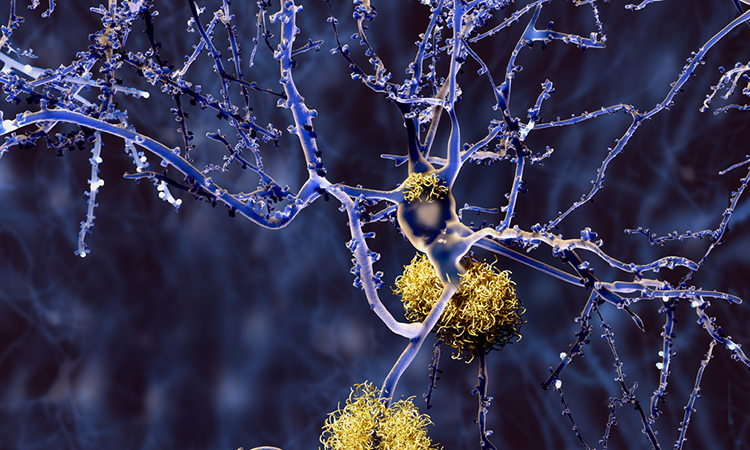
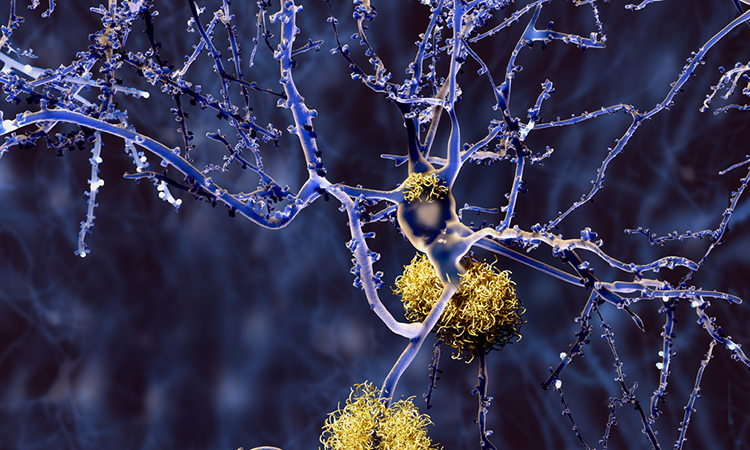
The A/T/N framework is accepted in research to categorise patients based on the presence of the three core biomarkers of the disease–amyloid, tau and neurodegeneration.4 Imaging, cerebrospinal fluid, and increasingly, blood-based tests can quantify these pathologies, helping researchers understand which patients may have or be at risk for Alzheimer’s disease.3
Use of the A/T/N framework has confirmed much of what we previously understood from carefully conducted longitudinal observational and post-mortem studies and helps translate that understanding into prospective clinical trials.5 We hope to advance the A/T/N framework from clinical trials to real-world settings for diagnosis and to guide patients along their treatment journey as more therapeutic options become available and, again, to ensure the right patient is treated with the right treatment at the right time.
What role do large biofluids proteomics datasets play in characterising the molecular processes that drive disease progression?
With Alzheimer’s disease and other neurodegenerative conditions, we know changes occur in a patient’s blood beyond the A, T and N.6 We also know that there are many different pathologies in the brain that can cause dementia beyond A, T and N, that may also be found in people with Alzheimer’s disease.7
Our hope is that large biofluids proteomics datasets can help us find biomarkers beyond A, T and N that facilitate precision intervention.8 These may also help in identifying or validating novel targets for therapy beyond A and T.8
In what ways does the integration of hypothesis-driven and hypothesis-free approaches enhance our ability to identify novel biomarkers and drug targets for Alzheimer’s disease?
“Integration” is the key word here, as we need both approaches to enhance identification of biomarkers and drug targets for Alzheimer’s disease. Hypothesis-driven work led us to identify beta amyloid and phosphorylated tau as both targets and biomarkers for Alzheimer’s disease.9
Hypothesis-free approaches, like the proteomics datasets mentioned above, may reveal biomarkers that had not been previously considered.
Today, with the help of these very large datasets and advanced analytics like machine learning (ML) and artificial intelligence (AI), we’re able to continue our investigations into unknown contributors to disease at a less expensive cost. As a researcher, it’s exciting to see how these innovations are bringing hope to patients, caregivers and loved ones impacted by Alzheimer’s disease.
What challenges remain in this area of research?
Although extensive progress has been made over the past few years, there is still so much we do not know. Continuing to expand our knowledge of biomarkers and identifying those that can complement A/T/N is critical for us to be able to better understand Alzheimer’s disease.
For example, patients with clinically diagnosed Alzheimer’s disease may also have other neurodegenerative pathologies. At post-mortem, pathologies involving alpha-synuclein and TDP43 are commonly observed in these patients but are not historically considered among the “cardinal” pathologies that define the disease.10,11 We need biomarkers of alpha-synuclein and TDP43 to complement the biomarkers we have today for A/T/N. As we improve our understanding of alpha-synuclein and TDP43, and how they contribute to disease progression, we will be able to better identify and target the right patients.12,13
Vascular disease is another pathology often accompanying Alzheimer’s disease, where it has been associated with cardiovascular and cerebrovascular risks.14
A well-known, and frequently studied component of Alzheimer’s pathology is inflammation.15 Over the past decade, in fact, the presence of inflammation has been associated with worsening of both tau and amyloid pathology, potentially representing a key step in the development of disease.15
One day, not before long, we hope to have A, T, N, a-synuclein, TDP43, vascular disease biomarkers, along with many others. A full complement of biomarkers accompanied by a full complement of therapies targeting different pathologies will be the promise of precision.
At Johnson & Johnson, our goal is to achieve this for diseases of the brain, moving beyond a “one-size-fits-all” diagnosis and treatment approach. Our scientists are dedicated to relentless innovation in biomarkers, data science, and clinical trials to identify disease subpopulations, tie targets of interest to disease development and presentation, and most importantly, leverage precision approaches to alleviate the burden of the many unmet needs across neuropsychiatric and neurodegenerative diseases.
References
- Juganavar, A., Joshi, A., & Shegekar, T. (2023, September 9). Navigating early alzheimer’s diagnosis: A comprehensive review of diagnostic innovations. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10561010/
- Devi, G. (2023, July 24). A how-to guide for a precision medicine approach to the diagnosis and treatment of alzheimer’s disease. https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2023.1213968/full
- Cummings J. The Role of Biomarkers in Alzheimer’s Disease Drug Development. Adv Exp Med Biol. 2019;1118:29-61. doi: 10.1007/978-3-030-05542-4_2. PMID: 30747416; PMCID: PMC6750734.
- Jack, C. R., Bennett, D. A., Blennow, K., Carrillo, M. C., Feldman, H. H., Frisoni, G. B., Hampel, H., Jagust, W. J., Johnson, K. A., Knopman, D. S., Petersen, R. C., Scheltens, P., Sperling, R. A., & Dubois, B. (2016, August 2). A/t/N: An unbiased descriptive classification scheme for alzheimer disease biomarkers. Neurology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4970664/
- Cousins, K. A. Q., Irwin, D. J., Wolk, D. A., Lee, E. B., Shaw, L. M. J., Trojanowski, J. Q., Da Re, F., Gibbons, G. S., Grossman, M., & Phillips, J. S. (2020, July 1). ATN status in amnestic and non-amnestic alzheimer’s disease and frontotemporal lobar degeneration. Brain: a journal of neurology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7364757/
- Yifei Lu, P. (2024, July 28). Changes in Alzheimer Disease Blood Biomarkers and Associations With Incident All-Cause Dementia. JAMA. https://jamanetwork.com/journals/jama/fullarticle/2821670
- Pugazhenthi, S. (2017, February 4). Metabolic syndrome and the cellular phase of alzheimer’s disease. Progress in molecular biology and translational science. https://pubmed.ncbi.nlm.nih.gov/28253987/
- Smets, Bart, et al. Large-scale proteomics to enable precision medicine for Alzheimer’s disease. Alzheimer’s Association International Conference; 2024 July 28 – August 1; Philadelphia, PA. Poster 362.
- National Institute of Aging. (2024, January 19). What happens to the brain in alzheimer’s disease? | National Institute on Aging. What Happens to the Brain in Alzheimer’s Disease? https://www.nia.nih.gov/health/alzheimers-causes-and-risk-factors/what-happens-brain-alzheimers-disease
- Li, K., Rashid, T., Li, J., Honnorat, N., Nirmala, A. B., Fadaee, E., Wang, D., Charisis, S., Liu, H., Franklin, C., Maybrier, M., Katragadda, H., Abazid, L., Ganapathy, V., Valaparla, V. L., Badugu, P., Vasquez, E., Solano, L., Clarke, G., Maestre, G., … Habes, M. (2023). Postmortem Brain Imaging in Alzheimer’s Disease and Related Dementias: The South Texas Alzheimer’s Disease Research Center Repository. Journal of Alzheimer’s disease : JAD, 96(3), 1267–1283. https://doi.org/10.3233/JAD-230389
- Josephs KA, Whitwell JL, Weigand SD, Murray ME, Tosakulwong N, Liesinger AM, Petrucelli L, Senjem ML, Knopman DS, Boeve BF, Ivnik RJ, Smith GE, Jack CR Jr., Parisi JE, Petersen RC, Dickson DW, 2014b. TDP-43 is a key player in the clinical features associated with Alzheimer’s disease. Acta Neuropathol127(6), 811–824.
- Meneses, A., Koga, S., O’Leary, J., Dickson, D. W., Bu, G., & Zhao, N. (2021, December 20). TDP-43 pathology in alzheimer’s disease. Molecular neurodegeneration. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8691026/
- Twohig, D., & Nielsen, H. M. (2019, June 11). Α-synuclein in the pathophysiology of alzheimer’s disease – molecular neurodegeneration. BioMed Central. https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-019-0320-x
- Lee, A. J. et al. (2022, May 24). FMNL2 regulates gliovascular interactions and is associated with vascular risk factors and cerebrovascular pathology in alzheimer’s disease – acta neuropathologica. FMNL2 regulates gliovascular interactions and is associated with vascular risk factors and cerebrovascular pathology in Alzheimer’s disease. https://link.springer.com/article/10.1007/s00401-022-02431-6
- Kinney, J. W., Bemiller, S. M., Murtishaw, A. S., Leisgang, A. M., Salazar, A. M., & Lamb, B. T. (2018, September 6). Inflammation as a central mechanism in alzheimer’s disease. Alzheimer’s & dementia (New York, N. Y.). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6214864/
About the author
Simon Lovestone, Vice President, Global Head, Neuroscience Discovery and Translational Science at Johnson & Johnson


His research interests include the identification of new targets for therapy in Alzheimer’s disease and related disorders through the understanding of basic mechanisms and clinical translation through experimental medicine and biomarkers; all this work underpinned by the use of Big Data ranging from molecular through to clinical information derived from electronic medical records.
Simon earned his bachelor’s degrees in microbiology from Sheffield University and in medicine from the University of Southampton, a Master of Philosophy in Clinical Research in Psychiatry and a doctorate in basic Neuroscience from the University of London and, until recently also practiced as a clinician in Old Age Psychiatry. He was Knighted for services to neuroscience in 2017 and was awarded an honorary degree by his alma mater, the University of Sheffield, in January 2022.
Related conditions
Alzheimer's disease (AD)
Related organisations
Johnson & Johnson
Related people
Simon Lovestone (Johnson & Johnson)



