Using clinical genomics and AI in drug development to elevate success
Posted: 11 February 2025 | Alessio Zoccoli, Carlos N Velez, Remco Jan Geukes Foppen, Vincenzo Gioia | No comments yet
How are clinical genomics and AI transforming drug development? Industry experts reveal how these technologies improve target identification, patient stratification, and trial design to drive higher success rates.


AI is revolutionising drug discovery, accelerating the development of novel treatments for cancer, neurological disorders, autoimmune diseases, and other hard-to-treat conditions.
Drug development: addressing complexity and success rates
Drug development is a complex and expensive process, requiring multidisciplinary expertise and high-risk financial investments. The major hurdles that pharmaceutical companies face are long lead times, high costs and a low probability of success (PoS). These hurdles not only delay patient access to innovative treatments but also threaten the economic sustainability of research and development (R&D) and the advancement of medical innovation.
The typical drug development journey spans a decade or more, encompassing distinct phases: discovery, preclinical research, clinical trials and regulatory approval. Each stage presents its own set of complexities and potential delays. The financial burden of drug development is substantial, often exceeding $2 billion per drug. Given that only a fraction of early-stage drug candidates progress to market, the costs associated with these failures are inevitably absorbed into the overall development costs. Addressing the long timelines and high costs of drug development is therefore critical for the advancement of medical innovation.
Unfortunately, many drug candidates fail. Clinical development failure may be due to an inability to demonstrate efficacy or sufficient safety.
Unfortunately, many drug candidates fail. Clinical development failure may be due to an inability to demonstrate efficacy or sufficient safety, or it may be due to other issues (such as unacceptable manufacturing procedures or efficiencies) that do not meet the requirements of the authorities. This failure is getting more pronounced by the day. Drugs that were developed and commercialised 30+ years ago were relatively simple small molecules. Today’s small molecules are far larger, more complex, and chase highly specific (and difficult to hit) targets, thereby increasing the chances of undesired side effects. Biologics have gone from monoclonal antibodies to complex bi- and tri-specific antibodies, as well as antibody-drug conjugates. Cell and gene therapies offer patients the possibility of living a relatively normal lifetime, with potential cures for deadly diseases.
The introduction of these new modalities comes at a significant financial cost and the probability of a drug candidate actually reaching approval and commercialisation is at historical lows. As recently as 2015, the likelihood of a drug in early clinical development achieving regulatory approval was around 25 percent. In 2021-2022, this ‘likelihood of approval’ (LOA) dropped below 6 percent, yet more recently they are returning to 10-11 percent, but still nowhere near what they used to be. Clearly, the more modern small molecules and other modalities are more difficult to develop, which is reflected in the LOA data. These failures not only increase overall costs, but also slow down scientific progress, delaying potential treatments for patients. Improving drug development success in the face of increasingly complex therapies is therefore a priority for the pharmaceutical industry.
Drug development has undergone a profound transformation, driven by technological innovations, regulatory and methodological changes, and the advent of new artificial intelligence (AI) technologies.
Very few drugs have been designed in recent years that have not benefitted from predictive models, or AI/ML models.
The application of AI in this field is a relatively new approach in drug discovery. However, computational methods have been heavily used in drug discovery since at least the 1990s, with machine learning (ML) tools and statistics-based models. Very few drugs have been designed in recent years that have not benefitted from predictive models, or AI/ML models. However, simply using AI for faster searches within existing and siloed datasets offers limited impact.
Fortunately, the sector is evolving towards a more integrated and sophisticated approach. This new methodology is based on the convergence between the analysis of vast clinical genomic datasets and the use of multimodal language models (MLMs). The ongoing transformation is leading to the gradual replacement of traditional processes with more dynamic and data-driven models, with the primary objective of improving clinical success rates and productivity.
New era in drug research: data access and NGS
The 1990s and 2000s marked a turning point in the drug development landscape, facilitated by a combination of cultural and technological factors that enabled regulatory changes, technological innovations and methodological advances.
Policy disruption and the surge of biomedical data
Since the 1990s, international policies have evolved, increasingly advocating for open access to biomedical data. These open access policies have unlocked vast repositories of clinical trial data, fuelling the growth of large-scale datasets that were previously inaccessible. This fosters a collaborative environment where academics, industry and regulatory institutions can jointly address drug development challenges. However, despite this progress, significant amounts of publicly funded data remain fragmented and unintegrated. These disconnected public datasets are in essence the antithesis of FAIR principles (Findable, Accessible, Interoperable, and Re-usable). Several pharma communities, including the Pistoia Alliance, are collaborating on FAIR implementation. Nevertheless, this disruptive policy empowers AI to leverage these immense datasets for training and discovery.
Accelerating genomic analysis and transforming clinical genomics
Introduced in the early 2000s, next-generation sequencing (NGS) revolutionised genomics by significantly accelerating the analysis of the human genome while dramatically reducing costs, compared to previous technologies. This technological advancement has enabled the discovery of genetic variants associated with various diseases, providing crucial insights into the molecular mechanisms underlying them. The speed and cost-effectiveness of NGS has empowered precision medicine within the context of clinical genomics.


AI’s power in drug discovery lies in its ability to revolutionise target identification, enhance patient stratification, and optimise trial design, driving higher success rates and faster access to life-saving treatments.
The role of clinical genomics in drug development
Before the era of clinical genomics, the choice of therapeutic targets was based mainly on empirical approaches and often incomplete biological hypotheses. Now, human genetic data is available that is associated with high quality disease data. For instance, one can now identify patients that have a disease linked to a certain mutation and determine a line of treatment. The recognised mutation-treatment interactions can help select patients for clinical trials and define treatments for patients that are already on the market.
The enormous amount of data generated in a short time by NGS equipment has led to the widespread adoption of clinical genomics in both industrial and hospital settings. Managing this data deluge requires the expertise of multidisciplinary fields like clinical bioinformatics, which bridges statistics, biology and computer science. Particular attention is given to the on-label and off-label clinical applications of new genomics-driven drugs.
The use of genomic and clinical data raises significant ethical issues related to the protection of patient privacy.
Clinical Bioinformatics plays a crucial role in managing this data deluge, including strategies to reduce data noise by pre-processing raw genomic data before feeding it to AI models. Furthermore, in terms of transparency and reproducibility of the results, the ability to reconstruct all the analytical steps that enable the raw unprocessed data to be transformed to the clinical report is fundamental. In the era of clinical genomics and AI, in fact, clinical reporting is strongly influenced by retrospective know-how and by the different levels of evidence between molecular alteration and target drug. The use of genomic and clinical data raises significant ethical issues related to the protection of patient privacy. The collection, storage and use of these data require secure technological infrastructures and transparent management policies to avoid the risk of privacy violations and discrimination. Furthermore, uneven access to genomic data amplifies inequalities in research.
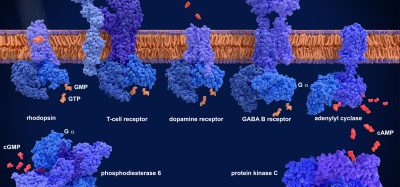
Clinical genomics enables the validation of therapeutic targets with greater precision, identifying genes and proteins directly implicated in disease mechanisms. Recent studies have shown that drugs developed on targets with strong genetic evidence have a greater PoS than those with unvalidated targets. Furthermore, the analysis of patient genomic profiles, combined with clinical and pharmacological data, can provide crucial information to improve the selection of drug candidates and the design of clinical trials. Clinical genomics has become particularly relevant in the development of new drugs based on generative AI thanks to its ability to provide a deeper understanding of disease biology, identify valid therapeutic targets, select predictive biomarkers of response and to stratify patients more precisely in an effort to impact PoS.
About the authors


Remco Jan Geukes Foppen, PhD, is an AI and life sciences expert specialising in the pharmaceutical sector. With a global perspective, he integrates and implements AI-driven strategies that impact business decisions, always considering the human element. His leadership has driven international commercial success in areas including image analysis, data management, bioinformatics, advanced clinical trial data analysis leveraging machine learning and federated learning. Remco Jan Geukes Foppen’s academic background includes a PhD in biology and a master’s degree in chemistry, both from the University of Amsterdam.






Literature
- Pallocca M, Betti M, Baldinelli S, et al. Clinical bioinformatics desiderata for Molecular Tumor Boards. Briefings in Bioinformatics, 2024, 25(5)
- Minikel E, Painter J, Dong C, Nelson M. Refining the impact of genetic evidence on clinical success. Nature 629, 624–629 (2024)
- Global Trends in R&D 2024: Activity, productivity, and enablers – Annual trend report from the IQVIA Institute for Human Data Science – Feb 22, 2024
- AI, PoS, and ROI: An alphabet soup of 21st Century drug development PART 2 In Life Science Leader by Remco Jan Geukes Foppen, Vincenzo Gioia and Carlos N. Velez (2024)
- AI, PoS, and ROI: An alphabet soup of 21st Century drug development PART 1 In Life Science Leader by Remco Jan Geukes Foppen, Vincenzo Gioia and Carlos N. Velez (2024)
- FDA DRAFT GUIDANCE: Considerations for the Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products
- Geukes Foppen RJ, Gioia V, Gupta S, et al. Methodology for Safe and Secure AI in Diabetes Management in Journal of Diabetes Science and Technology (2024).
Related topics
Artificial Intelligence, Drug Discovery, Drug Discovery Processes, Genomics, Next-Generation Sequencing (NGS)
Related people
Alessio Zoccoli, Carlos N Velez, Remco Jan Geukes, Vincenzo Gioia