Applications of molecular imaging in drug development
Posted: 25 July 2018 | Ben Burke (University of Hull and Castle Hill Hospital), Steve Archibald (University of Hull and Castle Hill Hospital) | No comments yet
The world of healthcare is rapidly evolving. With an ageing population, comes a significant increase in cancers, metabolic diseases and neurodegenerative disorders. New drug candidates are required; however drug development remains a lengthy and expensive process, with the average timeline now over 10 years and costs continuing to rise…


Medical imaging techniques provide non-invasive imaging of the body and can be used to track administered molecules (such as the drug candidates) or to use known radiotracers to report on biological processes that inform on the drug action or progression of the disease.
The use of molecular imaging in drug development is expanding.1 It has been a feature of preclinical development for many years, and the number of available radiotracers targeting biomarkers, which report on drug mechanism of action, has increased with an expanding knowledge of the biochemical processes in disease.2
After some high-profile drugs candidates not reaching approval, the desire to avoid late-stage failures in drug development is increasing and it is driving the interest in the use of molecular imaging. This is particularly relevant in the later stages of drug development to obtain accurate ‘in man’ pharmacokinetic and pharmacodynamic information, as well as reporting on biochemical or metabolic processes to determine efficacy.
Molecular imaging modalities
The key molecular imaging techniques for drug development are non-invasive and can be used to image the whole body. A molecular imaging modality must be highly sensitive to provide the level of information required to accurately track the molecules and the metabolites in vivo.
This means that the focus is on nuclear medicine and particularly positron emission tomography (PET). The high sensitivity and potential for quantification with PET makes it the modality of choice and, clinically, it is combined with computed tomography (CT) scanning that gives the anatomic data for co-registration (Figure 1). There is an ongoing and significant expansion of PET infrastructure (cyclotrons, radiopharmacies and PET / CT scanners) worldwide, increasing the relevance of these techniques. Single photon emission computed tomography (SPECT) imaging is less sensitive and not appropriate for dynamic imaging but has been used in some applications.
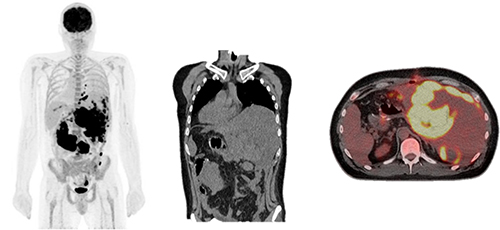
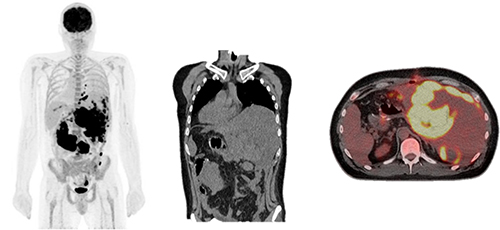
Figure 1: PET / CT image (left / right) showing the use of a biomarker to determine disease progression (a CT scan is shown in the middle).
There is also the potential for optical probe imaging to characterise skin diseases and other accessible areas of the body, as the tissue penetration is poor. It is an excellent technique for preclinical development but less relevant in the clinical setting.
The nuclear imaging techniques require the drug candidate (or the biomarker reporting radiotracer molecule) to be tagged with a radioisotope to allow detection. For a small molecule drug candidate, this will be a like-for-like replacement with a positron-emitting radioactive isotope of a carbon or fluorine atom. For immunotherapies, isotopes with a longer half-life are required and antibodies can be tagged with metal ion containing chelators (bioconjugation) without disruption of their activity.
Applications in oncology
The pharmacological audit trail (PhAT) has been recently proposed by Banerji and Workman in an attempt to address the significant costs associated with drug development by streamlining the process.3 The PhAT comprises key questions to be asked during development in which molecular imaging can offer significant information. Imaging can be used to demonstrate target engagement, tumour response and can give information on optimal treatment scheduling. Patients can subsequently be stratified for therapy based on target expression and whole body pharmacokinetic and pharmacodynamic profile.
Small molecule agents are often radiolabelled with commonly available short-lived organic radioisotopes carbon-11 (11C, t½ = 20 mins) or fluorine-18 (18F, t½ = 110 mins).4 The short half-lives of the isotopes overlap with the biological half-lives of the drugs. Carbon-11 radiolabelled analogues almost exclusively lead to radiotracers which are chemically identical to their carbon containing drug parents. Fluorine-18 agents are chemically very similar to their drug analogue, with fluorine often replacing a hydrogen atom if there is not a fluorine present in the molecular structure.
Monoclonal antibodies (mAbs) in cancer immunotherapy have emerged as an alternative strategy, with more than 20 now available for routine clinical use and hundreds more in clinical development. Molecular imaging is rapidly becoming essential in the development of new mAbs due to the significant variability in target expression and optimal dose.5 Monoclonal antibodies have a significantly longer biological half-life and, therefore, require an isotope with a longer physical half-life such as zirconium-89 (t½ = 78 hours), with work on the optimal strategy for isotope attachment an important research area.
Applications in neuroscience
Molecular imaging in drug development for neurological applications is early on in development, allowing for fast-tracking to clinical trials. As with all drug development projects, there is a need to streamline processes and reduce costs; molecular imaging is increasingly seen to support this effort. Drugs being designed for neurological applications are nearly exclusively small molecules and radiolabelled analogues are, therefore, carbon-11 or fluorine-18. PET imaging is often used to determine target occupancy and therapeutic effect as a fast-fail for drug candidates, for example, demonstration of target saturation without therapeutic effect or inadequate target occupancy would halt development and allow the focus of resources on other candidates. As a case study, Hoppin and co-workers presented Merck’s Substance P receptor (NK1R) probe [18F]SPARQ as an Aprepitant (Emend) analogue6 in which doses shown to saturate NK1R using PET were well below those required for an effect in trails for major depression.7-8 Alongside receptor saturation studies, molecular imaging can also be used in patient selection, to link post-mortem histopathology to patients and post-treatment evaluation of target density and brain function.
Molecular imaging has not yet been unequivocally shown to increase overall success rates from pre-clinical to launch in neuroscience but it can give clear information for either fast-tracking or fast-fail, allowing for focusing of resources on candidates with a higher chance of success. This can result in significant reduction of the financial burden.
Drug delivery applications
Another key area that can be optimised in drug development is the delivery of the compound to the target organ or tissue. Drug formulation and delivery / release profile are essential to ensure an effective drug candidate has optimal efficacy. These techniques can provide a new lease of life for drugs that have been used for many years is to improve the delivery profile.
However, delivery and release profiles are challenging to quantify and rely on indirect methods of detection – particularly in the developmental phase. These techniques are relevant for both oral and parenteral administration, however, an example of recent activity is pulmonary drug delivery through inhalers or nebulisers.9 In this case, many advances in formulation or delivery device design have been made to try to improve delivery parameters and efficacy but this is very challenging to validate. The industry still lacks the routine technology to determine this delivery profile in humans. There are some interesting advances in these areas and techniques for radiolabelling formulations and particles are being developed. In these applications, molecular imaging can have a key role in evaluating drug delivery in preclinical in vivo optimisation cycles prior to validation in humans using the same techniques.
Facilitating technology: microscale lab-on-a-chip / dose-on-demand technologies
There is a challenge in the use of molecular imaging technologies for clinical trials with the good manufacturing practices (GMP) production protocols that need to be developed for each molecule, which have the same degree of rigour as a commercial radiotracer. The use of an automated synthesis unit is required for GMP compliance and quality control protocols must be worked up and validated as a reproducible protocol, see top photograph. This is a barrier both to the use of radiolabelled molecule to allow ‘in-man’ pharmacokinetic studies and the development of a partner diagnostic, which could be used to advance the drug candidate to approval routine clinical use through robust patient selection protocols.
Microfluidic and lab-on-a-chip technologies offer advantages in highly efficient radiochemistry and the development of optimised synthetic routes. Making the radiolabelled molecule is one component of the process but there is also the quality control / validation methodology that must be completed in the PET radiopharmacy. From a regulatory perspective, the scale does not matter, the requirements are the same. Challenges then arise in the infrastructure required in the facility, for example, if a standardised HPLC method is needed this may require a dedicated instrument with the cost and space needed for this. Transfer of both synthetic and quality control steps to microfluidic lab-on-a-chip devices could result in cost savings and increased accessibility to the technology.10-11 This is also being extended to the production of lower cost particle accelerators (cyclotrons) to produce the radioisotope tags in either dedicated preclinical facilities or smaller ‘dose-on-demand’ radiopharmacies (Figure 2).12


Figure 2: A model for dose-on-demand PET radiotracer production with reduced infrastructure requirements.
Contract companies can provide fabrication of chip designs, which can be developed with scientific experts who have a good knowledge of optimal designs for radiochemistry after over 10 years of research activity in the development of lab-on-a-chip devices for radiotracer production.13-14 The quality control aspect is developing rapidly with some highly active research groups and commercial partners worldwide.15-16
Conclusion
With the increasing cost of drug development and the concurrent magnification of the risks of a late stage fail for pharma, there is a valid justification for the use of molecular imaging technologies in the preclinical phase to obtain pharmacokinetic/ pharmacodynamic data on the drug candidate. This can then transfer to late-phase clinical development to mirror this data in man, and to potentially provide a surrogate marker of response. These technologies can be expensive to apply and require expertise from radiochemistry through to data modelling.
Recent technological developments will facilitate the use of molecular imaging in drug development and, as the value has clearly been demonstrated, there will be an increase in both the underpinning research activity and services available from commercial research organisations with the facilities to drive these studies efficiently.
Biographies




References
- Matthews, PM; Rabiner, EA; Passchier, J; Gunn, RN, Positron emission tomography molecular imaging for drug development. British Journal of Clinical Pharmacology 2012, 73 (2), 175-186.
- Vavere, AL; Scott, PJH, Clinical Applications of Small-molecule PET Radiotracers: Current Progress and Future Outlook. Seminars in Nuclear Medicine 2017, 47 (5), 429-453.
- Banerji, U; Workman, P, Critical parameters in targeted drug development: the pharmacological audit trail. Seminars in Oncology 2016, 43 (4), 436-445.
- Waaijer, SJH; Kok, IC; Eisses, B; Schroder, CP; Jalving, M; Brouwers, A H; Lub-de Hooge, MN; de Vries, EGE, Molecular Imaging in Cancer Drug Development. Journal of Nuclear Medicine 2018, 59 (5), 726-732.
- Jauw, YWS; Menke-van der Houven van Oordt, CW; Hoekstra, OS; Hendrikse, NH; Vugts, DJ; Zijlstra, JM; Huisman, MC; van Dongen, G, Immuno-Positron Emission Tomography with Zirconium-89-Labeled Monoclonal Antibodies in Oncology: What Can We Learn from Initial Clinical Trials? Frontiers in Pharmacology 2016, 7.
- Patel, S; Schmidt, K; Hesterman, J; Hoppin, J, Advancing Drug Discovery and Development Using Molecular Imaging (ADDMI): an Interest Group of the World Molecular Imaging Society and an Inaugural Session on Positron Emission Tomography (PET). Molecular Imaging and Biology 2017, 19 (3), 348-356.
- Bergstrom, M; Hargreaves, RJ; Burns, HD; Goldberg, MR; Sciberras, D; Reines, SA; Petty, KJ; Ogren, M; Antoni, G; Langstrom, B; Eskola, O; Scheinin, M; Solin, O; Majumdar, AK; Constanzer, ML; Battisti, WP; Bradstreet, TE; Gargano, C; Hietala, J, Human positron emission tomography studies of brain neurokinin 1 receptor occupancy by aprepitant. Biological Psychiatry 2004, 55 (10), 1007-1012.
- Keller, M; Montgomery, S; Ball, W; Morrison, M; Snavely, D; Liu, G H; Hargreaves, R; Hietala, J; Lines, C; Beebe, K; Reines, S, Lack of efficacy of the substance P (neurokinin(1) receptor) antagonist aprepitant in the treatment of major depressive disorder. Biological Psychiatry 2006, 59 (3), 216-223.
- Darquenne, C; Fleming, JS; Katz, I; Martin, AR; Schroeter, J; Usmani, OS; Venegas, J; Schmid, O, Bridging the Gap Between Science and Clinical Efficacy: Physiology, Imaging, and Modeling of Aerosols in the Lung. Journal of Aerosol Medicine and Pulmonary Drug Delivery 2016, 29 (2), 107-126.
- Archibald, S; Pamme, N; Brown, N; Tarn, M, Integrated microfluidic lab-on-a-chip systems for F-18 radiotracer synthesis, purification and quality control. Journal of Nuclear Medicine 2015, 56 (3).
- Tarn, M. D.; Maneuski, D.; Alexander, R.; Brown, N. J.; O’Shea, V.; Pimlott, S. L.; Pamme, N; Archibald, SJ, Positron detection in silica monoliths for miniaturised quality control of PET radiotracers. Chemical Communications 2016, 52 (45), 7221-7224.
- Awasthi, V; Watson, J; Gali, H; Matlock, G; McFarland, A; Bailey, J; Anzellotti, A, A “dose on demand” Biomarker Generator for automated production of F-18 F- and F-18 FDG. Applied Radiation and Isotopes 2014, 89, 167-175.
- Lebedev, A; Miraghaie, R; Kotta, K; Ball, CE; Zhang, J Z; Buchsbaum, MS; Kolb, HC; Elizarov, A, Batch-reactor microfluidic device: first human use of a microfluidically produced PET radiotracer. Lab on a Chip 2013, 13 (1), 136-145.
- Lee, CC; Sui, GD; Elizarov, A; Shu, CYJ; Shin, YS; Dooley, AN; Huang, J; Daridon, A; Wyatt, P; Stout, D; Kolb, HC; Witte, ON; Satyamurthy, N; Heath, JR; Phelps, ME; Quake, SR; Tseng, HR, Multistep synthesis of a radiolabeled imaging probe using integrated microfluidics. Science 2005, 310 (5755), 1793-1796.
- Ha, NS; Sadeghi, S; van Dam, RM, Recent Progress toward Microfluidic Quality Control Testing of Radiopharmaceuticals. Micromachines 2017, 8 (11).
- Ly, J; Ha, NS; Cheung, SL; van Dam, RM, Toward miniaturized analysis of chemical identity and purity of radiopharmaceuticals via microchip electrophoresis. Analytical and Bioanalytical Chemistry 2018, 410 (9), 2423-2436.
The rest of this content is restricted - login or subscribe free to access


Why subscribe? Join our growing community of thousands of industry professionals and gain access to:
- quarterly issues in print and/or digital format
- case studies, whitepapers, webinars and industry-leading content
- breaking news and features
- our extensive online archive of thousands of articles and years of past issues
- ...And it's all free!
Click here to Subscribe today Login here
Related topics
Drug Delivery, Drug Development, Imaging, Neurosciences, Oncology, Technology