“Monumental” step in using human iPSCs towards treating complication of diabetes
Posted: 15 March 2022 | Ria Kakkad (Drug Target Review) | No comments yet
A new study led by the Indiana University School of Medicine showed human induced pluripotent stem cells can improve visual acuity, vascular health and other complications related to type 2 diabetes.
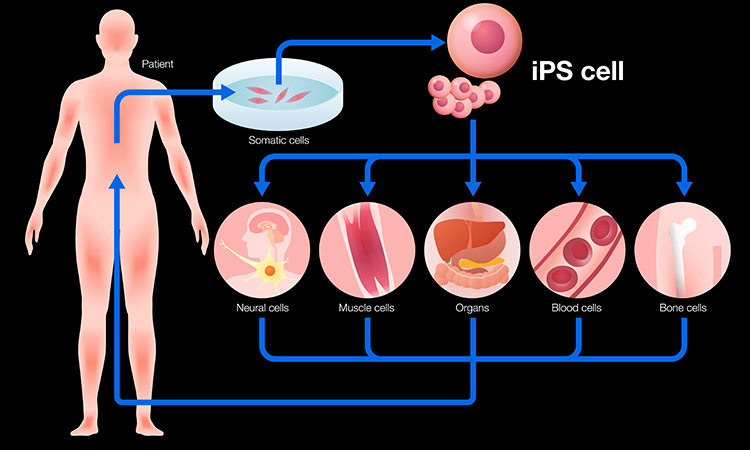
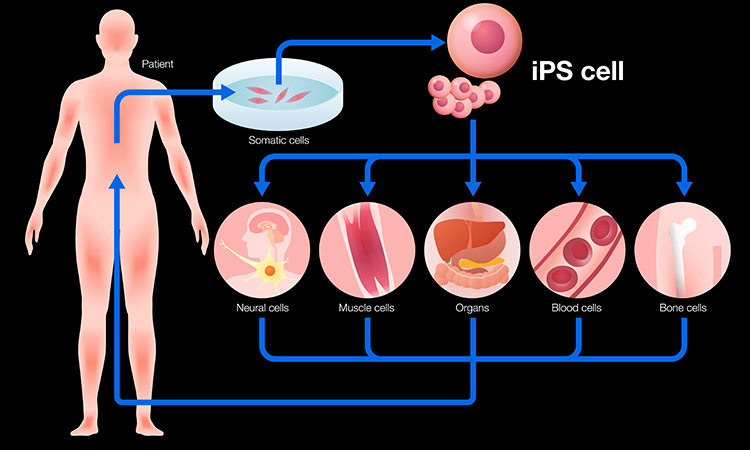
Researchers at the Indiana University School of Medicine, US have been investigating new regenerative medicine approaches to manage vascular health complications from type 2 diabetes. In collaboration with the University of Alabama at Birmingham, US and five other institutions, the team genetically reprogrammed diabetic and non-diabetic peripheral blood cells into human induced pluripotent stem cells (hiPSCs) and matured the cells into special blood vessel reparative cells. The study was recently published in Science Advances.
After injecting type 2 diabetic murine (T2D) retinal dysfunction into animal models, results showed significant improvement in visual acuity and electroretinograms with restoration of vascular perfusion. The researchers hypothesised hiPSC-derived vascular reparative cells may serve as a source of endothelial precursors that will display in vivo vessel reparative properties in diabetes subjects.
“Unlike the use of embryonic stem cells (ESCs), genetically engineered hiPSCs do not carry the ethical challenges ESCs possess that limit their possible usage and hiPSCs are being increasingly recognised as a viable alternative in study design and application as a cell therapy for human disorders,” said Dr Chang-Hyun Gil, first author of the study. “Our results demonstrate the safe, efficient and robust derivation of hiPSC-derived specific mesoderm subset for use as a novel therapy to rescue ischemic tissues and repair blood vessels in individuals with vascular diseases. The results provide a foundation for an early phase clinical trial.”
Researchers converted hiPSC into a specific mesoderm subset that was enriched to generate endothelial cells with vessel reparative properties similar to endothelial colony forming cells (ECFC).
The researchers found that the specific mesoderm subset expressing KDR, NCAM1 and APLNR (KNA+ mesoderm) exhibits enhanced capacity to differentiate into ECFC and form functional blood vessels in vivo and that mesoderm populations correct vasodegeneration of injured retinal vessels. Electroretinograms indicate enhanced function of neural retina and optokinetic nystagmus studies show improved vision.
The next translational step of the work for diabetes is to transfer the research protocols reported for differentiation of the hiPSC into to S–KNA+ cells into large scale manufacturing processes.
Related topics
Drug Targets, In Vivo, Induced Pluripotent Stem Cells (iPSCs), Stem Cells, Therapeutics, Translational Science
Related conditions
diabetes-related eye disease, Type-2 diabetes
Related organisations
Indiana University School of Medicine, The University of Alabama at Birmingham
Related people
Dr Chang-Hyun Gil








