Placenta’s role in genetic risk of schizophrenia
Posted: 25 May 2023 | Taylor Mixides (Drug Target Review) | No comments yet
A recent study led by the Lieber Institute for Brain Development has revealed that over 100 genes associated with the risk of schizophrenia appear to contribute to the development of the illness primarily through their influence on the placenta.


A recent study led by the Lieber Institute for Brain Development, US, has revealed that over 100 genes associated with the risk of schizophrenia appear to contribute to the development of the illness primarily through their influence on the placenta.
Until recently, scientists held a longstanding belief for more than a hundred years that genes associated with the risk of schizophrenia primarily pertained to the brain, and perhaps solely. However, a recent study published in Nature Communications, has unveiled a previously underestimated influence of the placenta in the progression of this disorder.
“The secret of the genetics of schizophrenia has been hiding in plain sight—the placenta, the critical organ in supporting prenatal development, launches the developmental trajectory of risk,” added Dr Daniel Weinberger, enior author of the paper and Director and CEO of the Lieber Institute for Brain Development, located on the Johns Hopkins medical campus in Baltimore. “The commonly shared view on the causes of schizophrenia is that genetic and environmental risk factors play a role directly and only in the brain, but these latest results show that placenta health is also critical.”
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
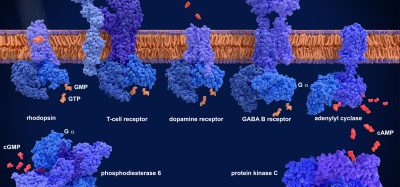
The study revealed that genes associated with schizophrenia have an impact on a crucial function of the placenta, which involves detecting nutrients in the mother’s bloodstream, including oxygen, and facilitating the exchange of nutrients accordingly. These genes exhibit lower levels of expression in the trophoblast cells, which form the core of the maternal-foetal nutrient exchange in the placenta. This diminished expression negatively affects the placenta’s ability to support the development of the foetus.
Furthermore, the research paper identifies several genes within the placenta that contribute to the development of conditions such as diabetes, bipolar disorder, depression, autism, and attention deficit hyperactivity disorder (ADHD). Nevertheless, the scientists discovered a notably higher number of genetic associations between schizophrenia and these genes compared to the other disorders mentioned.
“Targeting placenta biology is a crucial new potential approach to prevention, which is the holy grail of public health,” said Dr Gianluca Ursini, the lead author on the paper and an investigator at the Lieber Institute. “Scientists could detect changes in placental risk genes decades before the possible onset of a disorder, possibly even in the mother’s bloodstream during pregnancy. If doctors knew which children were most at risk of developmental disorders, they could implement early interventions to keep them healthy.”
Furthermore, the researchers came across concerning findings related to pregnancies affected by COVID-19. They examined a limited sample of placentas from mothers who had contracted COVID-19 during pregnancy and found a significant activation of the risk genes for schizophrenia within these placentas. This finding suggests that COVID-19 infection during pregnancy could potentially be a risk factor for schizophrenia due to its impact on the placenta. Scientists at the Lieber Institute are further exploring this possibility through NIH-funded research focused on studying COVID-19-affected placentas in order to gain deeper insights.
The researchers at the Lieber Institute are optimistic that their ongoing investigation into the placental genes will eventually result in the development of novel treatment and diagnostic methods, potentially bringing about a revolutionary transformation in the field of prenatal medicine. Their aspirations lie in harnessing the knowledge gained from studying these genes to create innovative tools that can enhance the accuracy and effectiveness of prenatal care in the future.
“In the modern era of molecular and genetic medicine, the standard treatment for a complicated pregnancy is still primarily bedrest,” says Weinberger. “These new molecular insights into how genes related to disorders of the brain and other organs play out in the placenta offer new opportunities for improving prenatal
Related topics
Antibodies, Covid-19, Drug Discovery, Drug Discovery Processes, Genomics, Targets
Related conditions
ADHD, Covid-19, Schizophrenia
Related organisations
Johns Hopkins medical campus, Lieber Institute for Brain Development (LIBD)
Related people
Daniel Weinberger, Gianluca Ursini