Potential biomarker found for inflammatory bowel disease
Posted: 6 December 2023 | Drug Target Review | No comments yet
A new approach called reverse metabolomics has discovered molecules that may serve as a biomarker or a therapeutic target for IBD.
Researchers at the University of California San Diego have developed a novel approach named “reverse metabolomics.” This technique combines organic synthesis, data science and mass spectrometry to investigate the molecules secreted by the microbiome and how they impact human health.
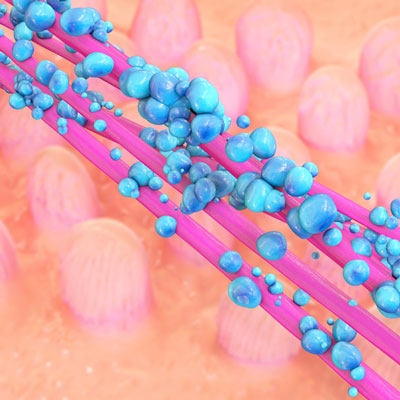
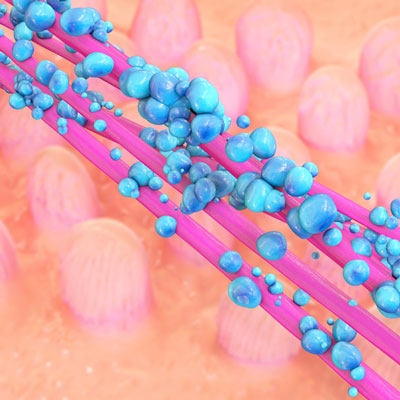
Microbiome research has begun to move its focus from the microbes themselves to the molecules they produce, which directly interact with human cells to affect a person’s health. However, attempting to find which molecules are being made by a person’s microbiome is difficult, as a typical metabolomics study can only characterise about 10 percent of the molecular data from a human microbiome sample.
In the new study, the scientists discovered hundreds of molecules that had never previously been observed in the human body in their first application of reverse metabolomics. A new metabolomic signature for inflammatory bowel disease (IBD) was identified using this new data. The scientists said these molecules may serve as a biomarker for diagnosing IBD, or as a possible therapeutic target to assist disease treatment.
Senior author Dr Pieter Dorrestein, Professor at Skaggs School of Pharmacy and Pharmaceutical Sciences at UC San Diego, said: “We know the microbiome is important, but we don’t know what kinds of molecules the microbes produce or how influential they are in the human body…Reverse metabolomics helps us evaluate whether specific molecules can be found in the samples, predict which microbes are producing them, and relate these metabolomic signatures to health and disease.”
Metabolomics
A tool called mass spectrometry is used to find different molecules in a sample in a typical metabolomics study. In this technique, each molecule has its own “barcode” that it can be identified by, but scientists still need to know what these barcodes represent to describe the contents of a sample.
To do this, scientists in the Dorrestein Lab took a backward approach. First author Dr Emily Gentry, Assistant Professor at Virginia Tech, used organic synthesis to produce thousands of different synthetic molecules from four classes of interest. She then defined each of their barcodes.
“If you read a biology textbook, none of these molecules will be in it,”
Next, publicly available metabolomics data was utilised, including data previously collected through the Crohn’s & Colitis Foundation. The researchers searched for the new barcodes in that data and found 145 of the synthesised bile acids were present in biological samples from public data, 139 of which had never been described before.
“If you read a biology textbook, none of these molecules will be in it,” explained Dorrestein. “Not only are they new to our understanding of human physiology, they’re entirely new to science, which is pretty amazing.”
“As more metabolomics data becomes publicly available, reverse metabolomics will become even more informative.”
Gentry and her colleagues then compared the metabolomic signatures of samples from different patient populations and discovered a strong association between a synthesised class of microbial molecules called bile amidates, and IBD. This association was validated across multiple cohorts, upholding the idea that these molecules are likely involved in the pathology of IBD.
Dr Gentry said: “As more metabolomics data becomes publicly available, reverse metabolomics will become even more informative.”
Certain bile amidates were increased in patients with Crohn’s disease specifically when they had active symptoms, although, this was not true for patients with ulcerative colitis. Such patterns could be used to help differentiate and diagnose specific types of IBD.
New Therapeutics
Also, the scientists started to investigate how these molecules might change gut health. Further experiments revealed that multiple bile amidate compounds may promote gut inflammation by dysregulating T cell function. One microbial compound produced a six-fold increase of a key cytokine known to be involved in the pathogenesis of Crohn’s disease.
The authors state that the molecules they have described could inspire novel therapeutics for treating IBD. Patients could be treated with pills containing live microbes that secrete specific molecules, or drugs that inhibit the enzymes these disease-associated molecules interact with.
This study was published in Nature.
Related topics
Mass Spectrometry, Microbiome, Molecular Biology
Related conditions
Crohn’s disease, Inflammatory bowel disease (IBD), ulcerative colitis
Related organisations
Crohn’s & Colitis Foundation, University of California San Diego, Virginia Tech