Perivascular fibroblasts support glioblastoma tumours
Posted: 13 December 2023 | Drug Target Review | No comments yet
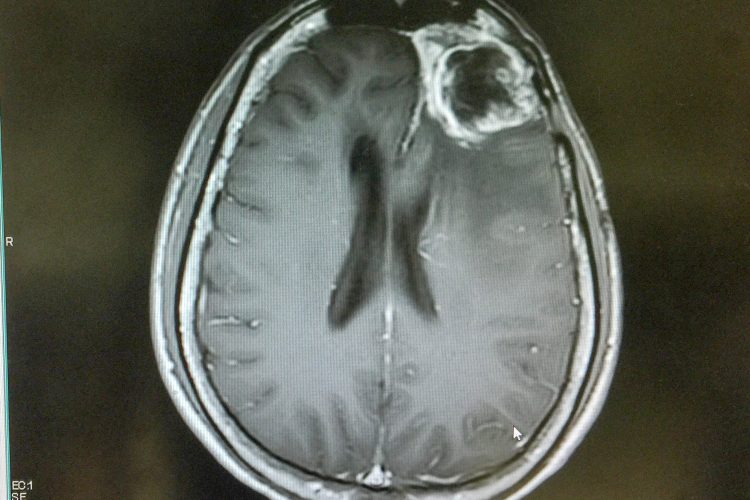
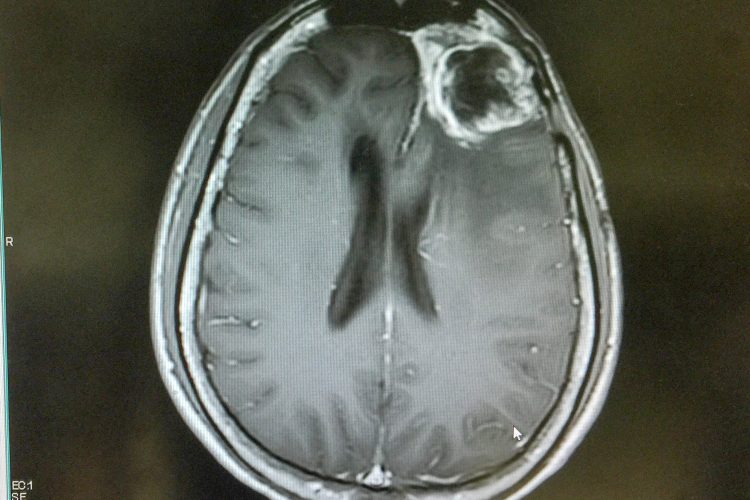
Glioblastomas can resist immunotherapy as perivascular fibroblasts support the creation of an immunosuppressive tumour environment.
Scientists at the University of Notre Dame have discovered that a largely understudied cell could provide a novel insight into how glioblastoma is able to resist immunotherapy.
Dr Meenal Datta, senior author of the study and Assistant Professor of aerospace and mechanical engineering at Notre Dame said: “A decade ago, we didn’t even know perivascular fibroblasts existed within the brain, and not just in the lining of the skull…My lab’s expertise is examining tumours from an engineering and systems-based approach and looking at the novel mechanical features in rare cancers that may have been understudied or overlooked.”
Dr Datta’s lab analysed different genes expressed in the tumour microenvironment related to the extracellular matrix using standard bioinformatics and AI-based approaches. The team found perivascular fibroblasts, which are normally found in the blood vessels of a healthy brain and deposit collagen to maintain the structural integrity and functionality of brain vessels.
Maksym Zarodniuk, a graduate student in Datta’s lab on the bioengineering doctorate programme, and first author on the study detailed: “We started in a completely different direction and stumbled upon this population of cells by using a combination of both bulk and single-cell RNA sequencing analyses of patient tumours.”
The data showed two groups of patients: those with a higher proportion of perivascular fibroblasts and those with significantly less. Brain cancer patients with more perivascular fibroblasts in their tumours were more likely to respond poorly to immunotherapies and have poor survival outcomes.
The team discovered that perivascular fibroblasts support the creation of an immunosuppressive tumour microenvironment, enabling the cancer to better evade the immune system. The fibroblasts may also help the cancer resist therapies, like chemotherapy that targets dividing cells, by promoting stem-like cancer cells that rarely divide. These are believed to be a major source of tumour relapse and metastasis.
Perivascular fibroblasts are a part of a healthy brain’s vasculature, so Datta thinks that these cells are breaking off and getting close to or infiltrating the glioblastoma tumour, but instead of supporting healthy brain function, they are being reprogrammed and helping the tumour.
“Most people think about the brain as being very soft, with soft cells and a soft matrix. But by putting down these fibroblasts and making these very fibrous proteins, it gives us an entirely different perspective on the structure of the brain and how it can be taken advantage of by cancer cells originating in the same organ,” Datta concluded.
This study was published in NPJ Genomic Medicine.
Related topics
Bioinformatics, Cancer research, Chemotherapy, Immunotherapy
Related conditions
Cancer Research, Glioblastoma
Related organisations
University of Notre Dame