Improved CAR T-cell immunotherapy for acute myeloid leukaemia
Posted: 14 February 2024 | Drug Target Review | No comments yet
Researchers have created dual-targeted CARs, which performed better than single-targeted CARs in both in vivo and in vitro experiments.
Scientists at St. Jude Children’s Research Hospital have improved chimeric antigen receptor (CAR) T–cell immunotherapy for acute myeloid leukaemia (AML). They overcame common issues with CAR T cells by using a small peptide to generate an additional means for the therapy to detect and eliminate cancer cells. Also, they used a computational approach incorporating AlphaFold predicted protein models to better understand how structure affects antigen recognition and therapy efficacy.
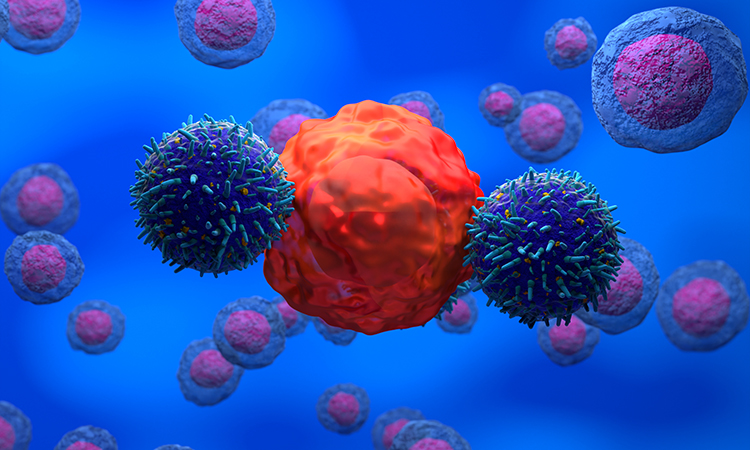
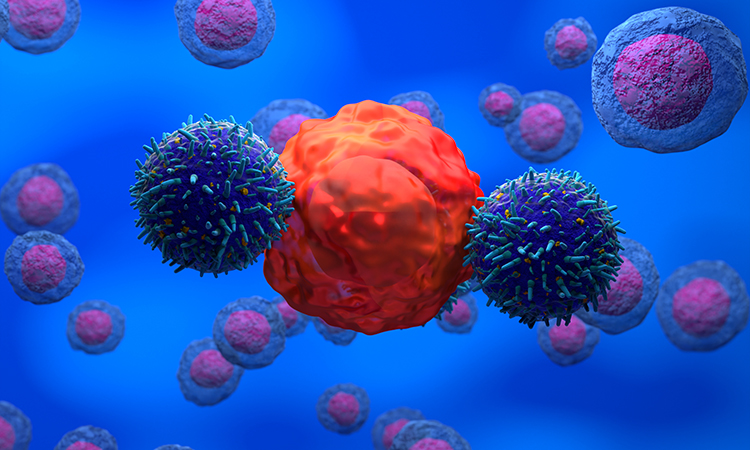
CAR T–cell therapy has been successful in treating some relapsed leukaemias. However, sometimes cancer cells that do not have the targeted protein can still grow, escaping the therapy and causing a relapse. The relapse rate for AML is high, resulting in an overall poor prognosis.
The St. Jude group believed it could be possible to combat this problem by targeting two different cancer-related proteins instead of one. Although others have tried a similar approach, they encountered problems with the structure of the bispecific CAR, so in the new study, the scientists added a small peptide to the CAR to act as the binder for the second targeted protein. They then confirmed their results with computational structural analysis of their improved constructs.
Senior corresponding author Dr Paulina Valasquez, from the St. Jude Department of Bone Marrow Transplantation and Cellular Therapy, commented: “One of the most exciting aspects of the study is that this approach can be widely extrapolated to other tumours…We focused on leukaemia, but combining bispecific CAR design with computational predictions can be widely extrapolated for other tumours such as solid and brain tumours.”
The new CAR is a single molecule, including the region of an antibody that binds its antigen and one short peptide that binds a separate target. A linker connects the two binding domains to enable binding of two different cancer-related proteins. First author Dr Jaquelyn Zoine, St. Jude Department of Bone Marrow Transplantation and Cellular Therapy, said: “We showed the value in finding creative ways to perform dual-antigen targeting…Prior bispecific CAR approaches use two antibody-based single-chain variable fragments, which are physically large molecules and can get in each other’s way, sometimes leading to poor or inefficient binding. Our approach instead added a small peptide, enabling our CAR to engage either platform to prevent immune escape.”
In both in vitro and in vivo experiments, the dual-targeted CARs performed better than single-targeted CARs, which shows promise for improving CAR T–cell function.
Co-author Dr M Madan Babu, St. Jude Center of Excellence for Data-Driven Discovery director, and the George J Pedersen Endowed Chair in Biological Data Science in the Department of Structural Biology, added: “We showed a proof of principle to explain and potentially expand the CAR design repertoire…But then comes the challenge. How do we know what linkers to choose? How do we know how much physical flexibility is needed?”
Identifying what type of linkers were more common in effective therapies could lead to future improvement because the physical structure of the targeting molecule and its linker that bridges the two binding domains can cause internal interference, stopping binding to the targets on the cancer cell. Computational structure predictions and comparing structures with experimental results confirmed that shorter, more flexible linkers would work better in the models.
Dr Babu explained: “We found when you have a linker of sufficient flexibility and shorter length so it doesn’t fold onto itself, it can scan a much larger volume and is more likely to find the target proteins on the cancer cell.”
Dr Kalyan Immadisetty, St. Jude Department of Bone Marrow Transplantation and Cellular Therapy and second author, said: “We are one of few groups in the world to use AI-based structure prediction tools for CAR design.” He confirmed the association between short, flexible linkers and greater anti-cancer efficacy by comparing 3D-modelled structures. This information supported the performance of the CAR in real experimental outputs.
Dr Immadisetty concluded: “Most importantly, others can now use our computational approach for designing their CARs…And hopefully, it will help them understand the efficacy of their CAR technology and lead to overall improvements for leukaemia and other malignancies.”
This study was published in Cell Reports Medicine.
Related topics
Cancer research, Chimeric Antigen Receptors (CARs), Computational techniques, Immunotherapy, In Vitro, In Vivo, Peptide Therapeutics
Related conditions
acute myeloid leukaemia (AML), Cancer Research
Related organisations
St Jude Children’s Research Hospital