New algorithm identifies high-risk precancerous lesions
Posted: 7 March 2024 | Drug Target Review | No comments yet
Researchers have developed an algorithm which could improve diagnostics of ovarian high-grade serous carcinoma.
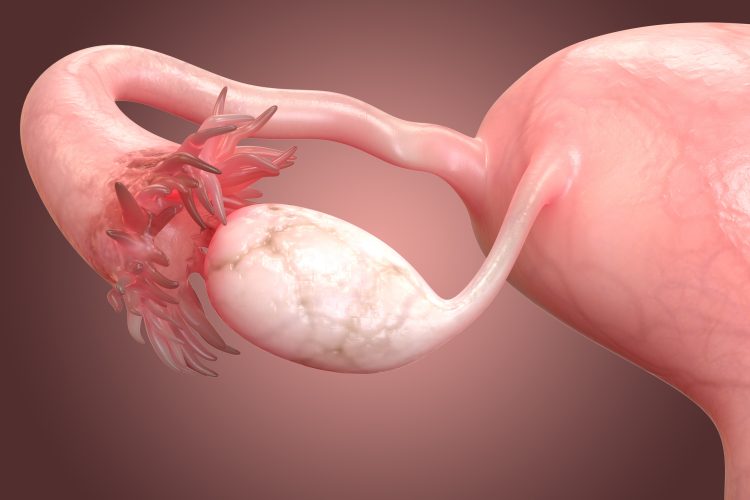
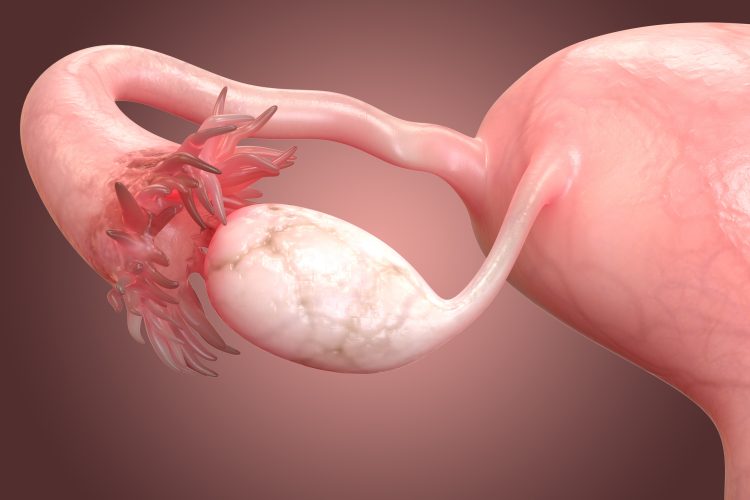
An algorithm to identify serous tubal intraepithelial carcinomas (STICs) on the fallopian tubes, considered the main precursors of ovarian high-grade serous carcinoma (HGSC), has been developed by scientists at the Johns Hopkins Kimmel Cancer Center and the Department of Gynecology and Obstetrics at the Johns Hopkins University School of Medicine. The study’s findings provided the first molecular evidence that STICs have unique identifiable genetic features, which could result in better diagnostics and improved outcomes.
Precursor lesions
Dr Ie-Ming Shih, Richard W. TeLinde Distinguished Professor and professor of gynaecology and obstetrics at the Johns Hopkins University School of Medicine, noted that women at an increased or average risk of developing ovarian cancer often undergo salpingectomy, but current clinical practice does not include a detailed examination of potential precancerous lesions.
One of the study’s lead authors, Dr Christopher Douville, assistant professor of oncology at the Johns Hopkins University School of Medicine, added: “This is a high-risk setting — these patients need more immediate diagnostic approaches…This test is about identifying precursor lesions before they progress to cancer.”
However, it is difficult to identify aggressive STICs early as not all STICs are molecularly equal. Therefore, the team aimed to develop a tool that could detect and stratify STICs according to key genetic alterations and mutations. Using a technique called Repetitive Element AneupLoidy Sequencing System (RealSeqS), the team sequenced 150 DNA samples and analysed the level of aneuploidy, the presence of missing or extra DNA chromosomes, in STIC versus HGSC and normal-appearing samples.
Initial results demonstrated that while normal-appearing samples had low levels of aneuploidy, STICs had significantly more non-random genetic alterations, even when they appeared structurally normal. This included whole and partial deletions of chromosome 17 in the signatures of the tumour suppressor p53 proteins.
The researchers suggest that the loss of chromosome 17 offers a possible explanation for the concurrent inactivation of both the TP53 and BRCA1 genes, which are both located on chromosome 17 and represent the most important tumour suppressors known to be involved in the development of HGSC. This could also explain why germline mutations involving the BRCA1 gene, and not BRCA2 (found in chromosome 13), are associated with a high risk of HGSC.
REAL-FAST
Based on these findings, the REAL-FAST algorithm was built to classify samples into distinct molecular groups, independent of their structural characteristics. It identified five groups, including a STIC subgroup with unique chromosome alterations that are associated with increased proliferation and abnormal growth.
Further validation of REAL-FAST for detecting STICs and HGSCs demonstrated that the test accurately detected the presence of cancer 95.8 percent of the time and correctly ruled out cancer where it did not occur 97.1 percent of the time. Together, the findings suggest that only some STICs progress to HGSC and that this progression is associated with a non-random increase in chromosomal abnormalities.
“The analysis of the RealSeqS data provides a basis for answering fundamental questions pertinent to the earliest events of HGSC development,” explained Dr Douville. “Although it can easily take a decade to translate research to clinical practice, Dr Shih feels this research could make a rapid impact on patient care by providing clinicians with diagnostic alternatives with quantitative answers.”
This study was published in Clinical Cancer Research.
Related topics
Artificial Intelligence, Cancer research, DNA, Oncology
Related conditions
Cancer Research, High-grade serous ovarian cancer (HGSC)
Related organisations
Johns Hopkins Kimmel Cancer Center, Johns Hopkins University School of Medicine.