Atlas of the human ovary offers huge potential for new treatments
Posted: 9 April 2024 | Drug Target Review | No comments yet
Single-cell RNA sequencing of ovaries resulted in the identification of four major cell types and four immune cell subtypes.
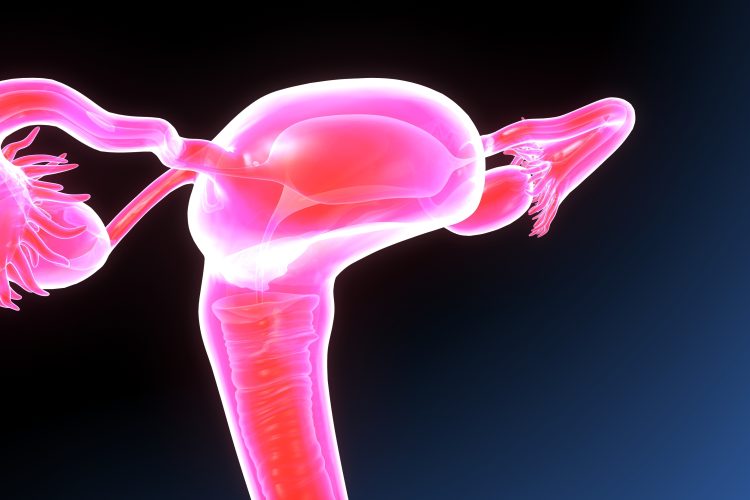
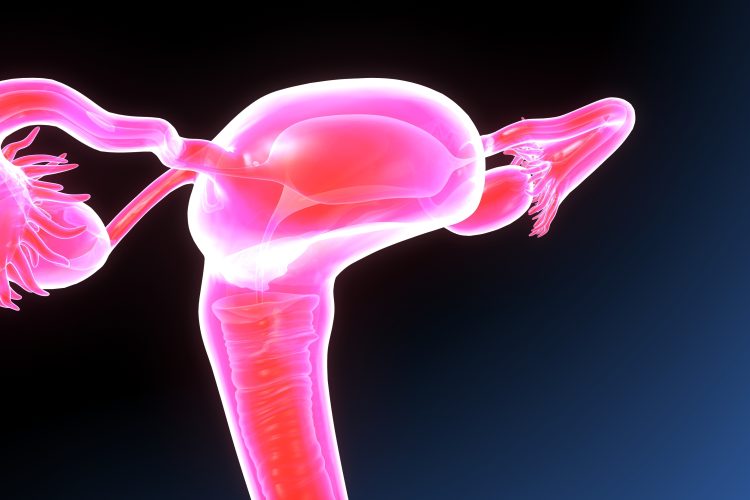
Researchers at the University of Michigan have created a new atlas of the human ovary, which provides insights that could lead to treatments, like developing artificial ovaries, to restore ovarian hormone production and the ability to have biologically related children.
The new atlas shows the factors that enable a follicle to mature, as most follicles die, without releasing hormones or an ovum. The team used new tools that can identify what genes are being expressed at a single-cell level within a tissue, to investigate ovarian follicles that carry the immature precursors of ovums, known as oocytes.
Dr Ariella Shikanov, corresponding author and UM associate professor of biomedical engineering, commented: “Now that we know which genes are expressed in the oocytes, we can test whether affecting these genes could result in creating a functional follicle. This can be used to create an artificial ovary that could eventually be transplanted back into the body.”
For this, tissues that were stored and frozen before exposure to toxic medical treatments like chemotherapy and radiation could be used. Presently, surgeons can implant previously frozen ovarian tissue to temporarily restore hormone and egg production, but this is not efficacious for a long period of time because very few follicles survive through reimplantation.
Most follicles, named primordial follicles, remain dormant and are found in the outer layer of the ovary, the cortex. A small number of these follicles activate periodically and migrate into the ovary, to a region termed ‘the growing pool’. Then, only a limited number of those growing follicles produce mature eggs that are released into the fallopian tube.
The team believes that, with the ability to guide follicle development and tune ovarian environment, engineered ovarian tissue could function for much longer than unmodified implanted tissue. This would result in a longer fertility window in patients, as well as a longer period in which their bodies produce hormones that help regulate the menstrual cycle and support muscular, skeletal, sexual and cardiovascular health.
Associate Chair of UM’s Department of Computational Medicine and Bioinformatics and co-corresponding author of the study Dr Jun Li, stated: “The magic we’re working toward is being able to trigger an immature cell into maturity, but without knowing which molecules drive that process, we’re blind.”
Using spatial transcriptomics, the researchers performed single-cell RNA sequencing of ovaries from five human donors, generating data for 21,198 cells, which resulted in the identification of four major cell types and four immune cell subtypes.
“This was the first time where we could target ovarian follicles and oocytes and perform a transcription analysis, which enables us to see which genes are active,” Dr Shikanov said. “The majority of ovarian follicles, already present at birth, never enter the growing pool and eventually self-destruct. This new data allows us to start building our understanding of what makes a good egg—what determines which follicle is going to grow, ovulate, be fertilised and become a baby.”
UM’s work is part of the Human Cell Atlas project, which seeks to understand different cells’ molecular characteristics and what goes wrong in disease.
This study was published in Science Advances.
Related topics
RNAs, Sequencing
Related conditions
infertility
Related organisations
Michigan University