How tumours prevent formation of immune responses
Posted: 25 April 2024 | Drug Target Review | No comments yet
Scientists found that preventing the effects of prostaglandin E2 could be an effective therapy to overcome tumour defence.
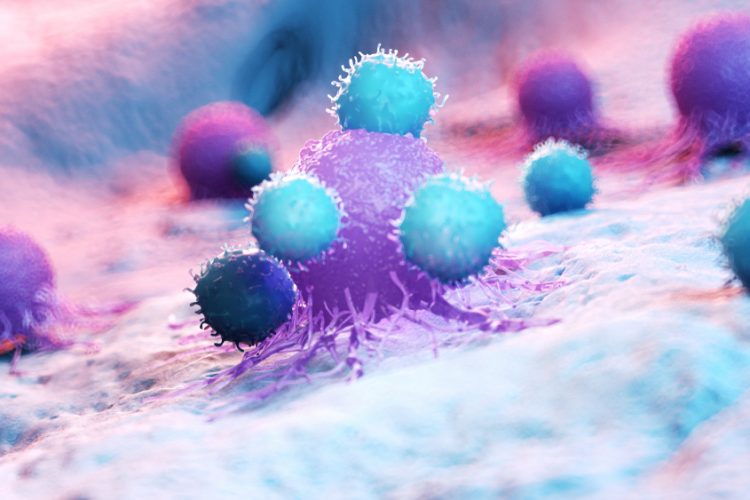
Researchers at the Technical University of Munich (TUM) and the Ludwig-Maximilians-Universität München (LMU) Hospital have discovered how tumours actively prevent the formation of immune responses by cytotoxic T cells. The study’s findings provide rationales for new cancer immunotherapies and could make existing treatments more effective.
Led by Dr Jan Böttcher, research group leader at the Institute of Molecular Immunology at TUM, and Professor Sebastian Kobold, Deputy Director of the Department of Clinical Pharmacology at LMU Klinikum München, the team found that tumours use a messenger substance to influence immune cells in an early phase of the immune response. Numerous cancer cells demonstrate increased secretion of the messenger substance prostaglandin E2. The researchers showed that prostaglandin E2 binds to EP2 and EP4, two receptors on the surface of certain immune cells.
These stem-like T cells migrate from other areas of the body into the tumour. They multiply in the tumour and develop into cytotoxic T cells that attack the cancer if the immune response is successful. Dr Böttcher elucidated: “This whole process is strongly limited when tumours secrete prostaglandin E2 and this factor binds to EP2 and EP4 receptors…The T cell response collapses and the tumour can progress.” If the interaction of messenger substance and receptor in tumour models is prevented, the immune system fought the tumours effectively.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
Dr Böttcher explained: “We have discovered a mechanism that influences the body’s immune response in a crucial phase…Many tumours prevent the stem-like T cells from generating cytotoxic T cells in the tumour that could attack the cancer.”
Current immunotherapies aim to prevent the cancer from switching off immune responses at a later phase. For example, checkpoint inhibitor therapies release the blockade of fully differentiated cytotoxic T cells and switch them back on. Before T cell exhaustion occurs, which other researchers are trying to stop, differentiated T cells must also be present.
“Current treatment approaches would probably be more effective if the effects of prostaglandin E2 on stem-like T cells is blocked to enable their unhindered differentiation within tumour tissue,” commented Professor Kobold. This also applies to recent approaches that need the protein IL-2 to stimulate T cells. It was shown that as soon as the prostaglandin E2 binds to the two receptors, T cells can no longer respond to IL-2. Dr Kobold added: “We suspect that even the body’s own IL-2 signals may be sufficient to enable T cells to successfully fight cancer once the effects of prostaglandin E2 have been stopped.”
“We now have a concrete starting point for significantly improving immunotherapies,” Dr Böttcher concluded. “Researchers around the world must now develop strategies to overcome the tumour’s defence. We need to stop the effects of prostaglandin E2 – either by preventing tumours from producing the molecule or by making immune cells resistant to it.”
This study was published in Nature.
Related topics
Cancer research, Immunotherapy, T cells
Related conditions
Cancer, Cancer Research
Related organisations
Ludwig-Maximilians-Universität München (LMU) Hospital, Technical University of Munich (TUM)
Related people
Dr Jan Böttcher (TUM), Professor Sebastian Kobold (LMU)