How gKetoC alleviates intestinal inflammation
Posted: 10 May 2024 | Drug Target Review | No comments yet
Through in vitro and in vivo models, researchers find a mechanism by which bacteria-generated fatty acids regulate immune responses.
Researchers at the Tokyo University of Science, led by Dr Chiharu Nishiyama have conducted a series of experiments using both in vitro and in vivo mouse models to understand how bacteria-generated fatty acids (FAs) regulate immune responses.
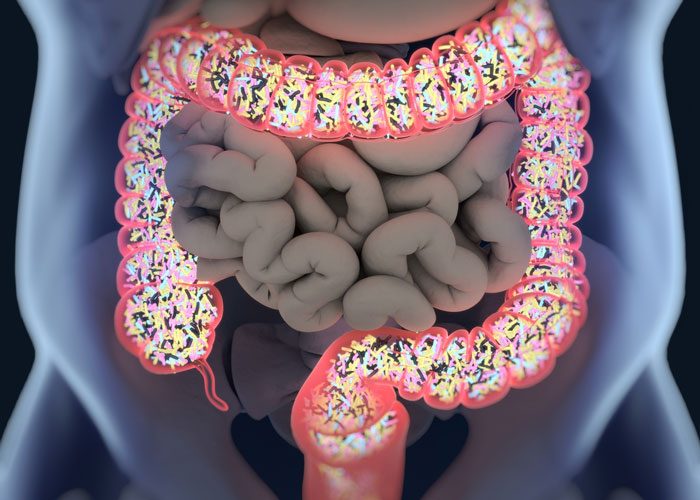
Intestinal microbiota plays a crucial role in digestion and maintenance of overall health, as they metabolise dietary components into beneficial fatty acids (FAs), supporting metabolism and maintaining host body homeostasis. Metabolites originating from polyunsaturated fatty acids (PUFAs), influenced by gut microbes like Lactobacillus plantarum, exhibit powerful effects on inflammation and immune responses. Therefore, manipulating gut bacteria and their metabolites offers promise for treating metabolic and inflammatory disorders, but the exact mechanisms controlling the immunomodulatory properties of microbe-derived metabolites are unknown.
Dr Nishiyama explained: “PUFAs undergo metabolic transformations such as hydroxylation and saturation by enzymes possessed by intestinal bacteria. In recent years, a variety of beneficial physiological effects have been discovered for these intestinal bacterial metabolites. In this study, we have investigated the activity of multiple FA metabolites using mouse-derived immune cells.”
Investigating molecular mechanisms
The scientists used antigen-stimulated spleen cells to prompt an enhanced immune response. They then investigated the impacts of different PUFA derivatives, focusing on metabolites of linoleic acid (LA). Their findings showed that KetoC, αKetoC, gKetoA, and gKetoC (enon derivatives of LA) notably reduced the levels of interleukin 2 (IL-2), a protein that initiates the expansion of immune cells and inflammation.
However, the original PUFAs in their unconverted form did not have the same immunosuppressive effects, emphasising the essential role of bacterial conversion in activating their immunomodulatory properties. Also, the team saw that the enon FAs suppressed prolonged T-cell proliferation and dendritic cell activation, which can result in inflammation and autoimmune diseases. This anti-inflammatory effect was most definite with gKetoC. Therefore, they aimed to elucidate the molecular mechanisms by which gKetoC applied its immunosuppressive effects.
Previous studies have shown the involvement of G protein-coupled receptors (GPCRs) and the transcription factor, NRF2, in antioxidant responses, which are mediated by numerous FA metabolites. However, the involvement of GPCRs and NRF2 in the effects of gKetoC in dendritic cells remained elusive. By assessing the levels of inflammatory cytokines released from antigen-stimulated and gKetoC-treated dendritic cells, the scientists clarified the role of these proteins in gKetoC-mediated immune responses.
The findings indicated that gKetoC stimulated the NRF2 signalling pathway, which suppressed the production of inflammatory cytokines. GPCR-signalling inhibited inflammatory cytokine production in dendritic cells in an NRF2-dependent manner, revealing a potential molecular axis governing the immunomodulatory effects of gKetoC.
gKetoC treatment
The researchers used a mouse model of inflammatory bowel disease (IBD) to further validate their results in vivo, examining immune and inflammatory responses by involving gKetoC treatment. gKetoC treatment significantly reduced fibrosis-induced tissue damage in the colon, reduced colitis-induced weight loss, and improved stool scores. Additionally, the treated mice demonstrated decreased epithelial cell disruption and ulcers, along with reduced infiltration of immune cells and lower serum levels of inflammatory factors. The models deficient in NRF2 showed substantial restoration of colitis-induced tissue damage after gKetoC treatment.
More research is required to understand the interplay between gKetoC, GPCR-signalling, and the NRF2 pathway, and uncover other potential targets of gKetoC. Dr Nishiyama concluded: “Our findings demonstrate that the compounds of dietary oils are converted into useful metabolites with anti-inflammatory effects by gut bacteria. By conducting detailed analyses at the individual, cellular, and genetic levels, we hope to understand how the food we eat daily influences the function of immune cells, and how these effects can be targeted for the prevention and mitigation of inflammatory diseases.”
The team believes that these developments could aid the identification and development of compounds that can prevent or alleviate immune related diseases.
This study was published in Frontiers in Immunology.
Related topics
Animal Models, Drug Targets, In Vitro, In Vivo
Related conditions
Colitis, Inflammatory bowel disease (IBD)
Related organisations
Tokyo University of Science
Related people
Dr Chiharu Nishiyama (Tokyo University of Science)