Macrophage-mediated phagocytosis: treating solid tumours
Posted: 4 June 2024 | Drug Target Review | No comments yet
A new immunotherapy approach combining co-engineered T cells and antibodies enhances phagocytosis of tumour cells.
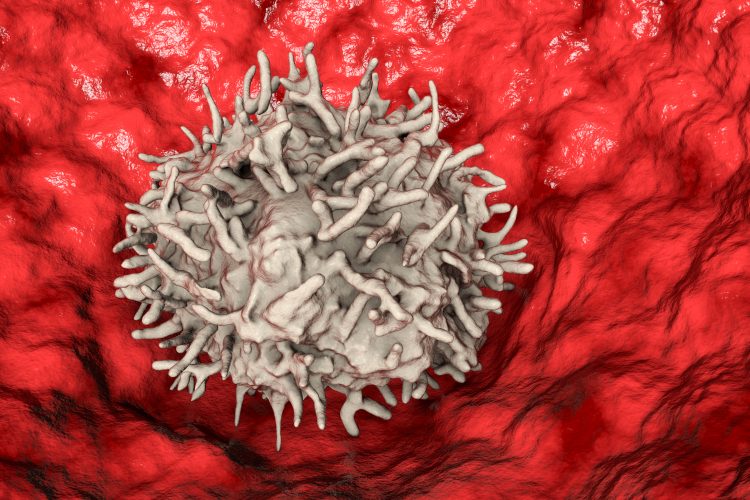
Scientists at Ludwig Cancer Research have developed a new immunotherapy approach which employs a two-pronged attack against solid tumours. The study concentrates on adoptive cell transfer (ACT).
Dr Melita Irving, from Ludwig Lausanne, led the study. She explained: “While T cell therapies have shown tremendous success in treating certain blood cancers, solid tumours present a more complex challenge due to immune-suppressive mechanisms at play in the tumour microenvironment…T cells alone may not be sufficient, which is why we’re exploring ways to boost their effectiveness by integrating other immune-enhancing strategies.”
Dr Irving and her colleagues modified T cells to secrete CV1, a high-affinity version of the human signal regulatory protein alpha (SiRPα). Typically, SiRPα interacts with CD47, a protein found on the surface of healthy cells that transmits a signal to prevent macrophages from engulfing them. However, many cancer cells manipulate this system by overexpressing CD47 to avoid being phagocytised.
A previously developed CV1 decoy utilised by the team binds CD47 with high affinity, silencing the phagocytosis signal. They expected this to make the cancer cells more recognisable and susceptible to macrophage attack. This was while the cancer cells were also being targeted by the engineered T cells, which had been co-engineered to express an affinity-optimised T cell receptor (TCR).
However, unexpectantly, the CV1 that the T cells were engineered to secrete included an Fc tail. These are normally located at the tail end of an antibody molecule and doubles as a tag that draws macrophage attack. With the tag coating the T cells secreting the engineered CV1, it prompted a macrophage assault on the therapeutic T cells, resulting in their depletion in treated mice.
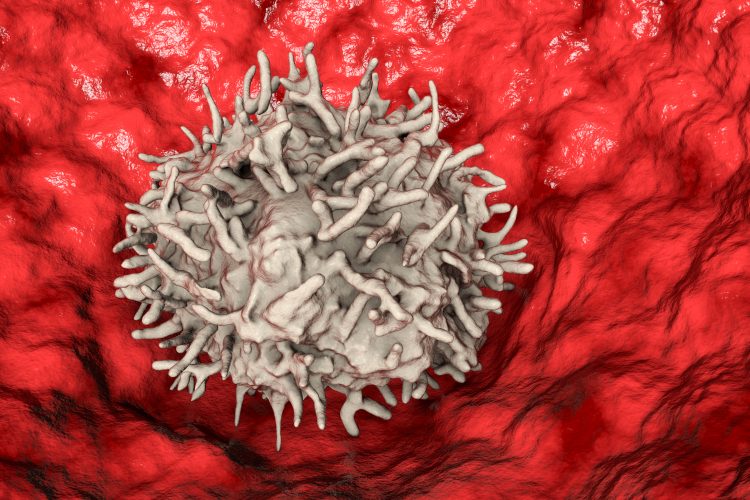
First author of the study Evangelos Stefanidis, a recent PhD graduate from Irving’s group, modified the T cells to express CV1 alone, without the Fc tail, which stopped the engineered T cells being targeted by human macrophages.
When the CV1-producing T cells were combined with cancer-targeting antibodies like Avelumab and Cetuximab, the macrophage’s ability to consume tumour cells was further improved. This was due to the antibodies, which target the immune-suppressing PD-L1 molecule and the growth-promoting Epidermal Growth Factor Receptor (EGFR), having active Fc tails that engage macrophages to attack the tumour cells specifically. As well as this, the researchers saw that treating mice with these antibodies altered the tumour microenvironment beneficially to support immune attack.
“By removing the Fc tail, we could spare the T cells from human macrophages, and by combining the co-engineered T cells with clinical antibodies comprising an active Fc tail, we specifically augmented phagocytosis of the tumour cells by macrophages,” Dr Irving commented.
Furthermore, these results could elucidate why clinical trials of the antibody drug magrolimab have faced great challenges, such as infections and poor patient responses. Like the CV1 decoy, magrolimab blocks the CD47 signal on tumour cells to encourage their destruction by the immune system. Yet, if its blocking action is not targeted only to cancer cells, like the CV1 decoys with Fc tails, it could cause the destruction of healthy tissues.
Dr Irving concluded: “It is possible that magrolimab is also targeting immune cells, including T cells, for phagocytosis…Our combination treatment strategy helps direct phagocytosis specifically against tumour cells while sparing our engineered T cells. Our findings also highlight the complexities of cancer treatment and the importance of a nuanced approach to immunotherapy.”
This study was published in the Journal of Clinical Investigation.
Related topics
Cancer research, Immunotherapy, In Vitro, T cells, Targets, Therapeutics
Related conditions
Cancer Research, solid tumours
Related organisations
Ludwig Cancer Research