New biological pathway in IBD discovered
Posted: 6 June 2024 | Drug Target Review | No comments yet
Researchers have identified a new biological pathway driving IBD and similar conditions that could be targeted with MEK inhibitors.
A new biological pathway that is a primary driver of inflammatory bowel disease (IBD) and similar conditions, which can be targeted with existing drugs, has been discovered by scientists at the Francis Crick Institute, UCL and Imperial College London.
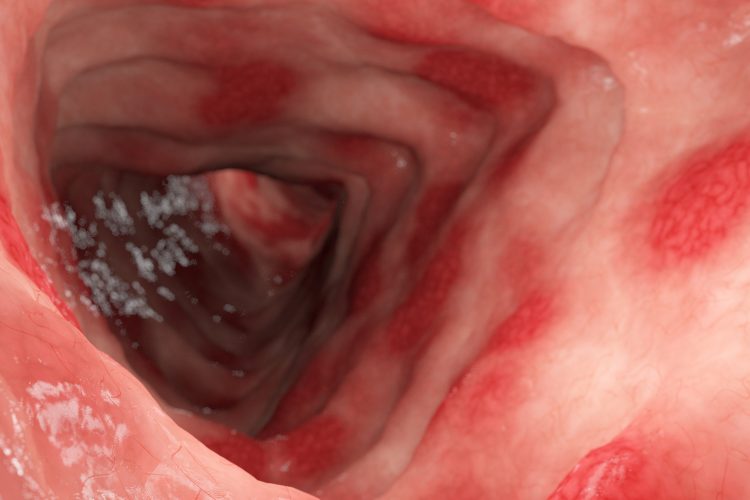
At present, around five percent of the global population are affected by an autoimmune disease, like IBD, the umbrella term for Crohn’s disease (CD) and ulcerative colitis (UC). These diseases are becoming more prevalent, but current treatments are not effective in every patient. A lack of understanding about the causes of IBD means that attempts to develop novel drugs frequently fail.
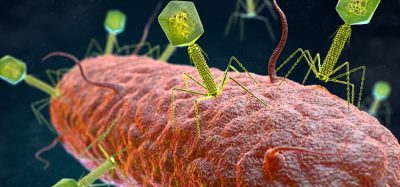
The team explored a ‘gene desert,’ an area of DNA that does not code for proteins, on chromosome 21. The gene desert has previously been associated with IBD and numerous other autoimmune diseases. They discovered that this gene desert contains an enhancer, which was only active in macrophages, an immune cell known to be significant in IBD. This enhancer boosted the ETS2 gene, with higher levels correlating with an elevated risk of disease.
With genetic editing, the team uncovered that ETS2 is crucial for almost all inflammatory functions in macrophages, including several that directly contribute to tissue damage in IBD. Notably, increasing the amount of ETS2 in resting macrophages altered them into inflammatory cells that closely resembled those from IBD patients. It was also found that other genes previously linked to IBD are part of the ETS2 pathway, providing further evidence that it is a key cause of IBD.
“Using genetics as a starting point, we’ve uncovered a pathway that appears to play a major role in IBD and other inflammatory diseases.”
Although specific drugs that block ETS2 do not exist, the researchers investigated drugs that might indirectly reduce its activity and predicted that MEK inhibitors, drugs already prescribed for other non-inflammatory conditions, could turn off the inflammatory effects of ETS2. Testing MEK inhibitors demonstrated reduced inflammation in macrophages, as well as in gut samples from patients with IBD.
Now the team are collaborating with LifeArc to determine methods to deliver MEK inhibitors directly to macrophages. James Lee, Group Leader of the Genetic Mechanisms of Disease Laboratory at the Crick, and Consultant Gastroenterologist at the Royal Free Hospital and UCL, who led the research, commented: “Using genetics as a starting point, we’ve uncovered a pathway that appears to play a major role in IBD and other inflammatory diseases. Excitingly, we’ve shown that this can be targeted therapeutically, and we’re now working on how to ensure this approach is safe and effective for treating people in the future.”
“This research is a really exciting step towards the possibility of a world free from Crohn’s and Colitis one day.”
Ruth Wakeman, Director of Services, Advocacy and Evidence at Crohn’s & Colitis UK concluded: “Every year, more than 25,000 people are told that they have Inflammatory Bowel Disease. Crohn’s and Colitis are complex, lifelong conditions for which there is no cure, but research like this is helping us to answer some of the big questions about what causes them. The more we can understand about Inflammatory Bowel Disease, the more likely we are to be able to help patients live well with these conditions. This research is a really exciting step towards the possibility of a world free from Crohn’s and Colitis one day.”
This study was published in Nature.
Related topics
Disease Research, Drug Repurposing, Drug Targets, Genome Editing, Therapeutics
Related conditions
Crohn’s disease (CD), Inflammatory bowel disease (IBD), ulcerative colitis (UC)
Related organisations
Crohn's & Colitis UK, Francis Crick Institute, Imperial College London, UCL