P. aeruginosa infection method elucidated with microtissue model
Posted: 10 June 2024 | Drug Target Review | No comments yet
Researchers found, using human respiratory epithelium organoids, that P. aeruginosa breaches respiratory epithelia by goblet cell invasion.
Researchers at the Biozentrum of the University of Basel have used human lung microtissues to reveal how Pseudomonas aeruginosa, a dangerous nosocomial pathogen that causes severe and life-threatening pneumonia, has developed a sophisticated method to infect the lungs. This study was conducted as part of the National Center of Competence in Research (NCCR) “AntiResist.”
Pseudomonas aeruginosa is resistant to numerous antibiotics and is particularly threatening to immunocompromised patients and those on mechanical ventilation, with mortality rates up to 50 percent. To discover new insights into the infection process, Dr Urs Jenal and his team used lab-grown lung microtissues generated from human stem cells.
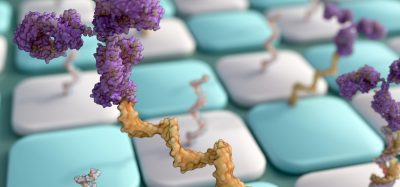
They observed that Pseudomonas breaches the top layer of lung tissue, a thin layer of tightly packed cells covered in mucus which traps microorganisms and then removes them with specialised cells. This is an almost impenetrable barrier, but Pseudomonas has been able to invade. Dr Jenal explained: “It uses the mucus-producing goblet cells as Trojan horses to invade and cross the barrier tissue. By targeting the goblet cells, which make up only a small part of the lung mucosa, the bacteria can breach the defence line and open the gate.”
Pseudomonas has many virulent factors, named secretion systems, attacking and invading the goblet cells. When inside the cells, they replicate, killing the cells. The eruption of the dead cells results in ruptures in the tissue layer, causing the protective barrier to become leaky. The pathogens exploit this weak spot, rapidly colonising at the rupture sites and spreading into deeper tissue regions.
Although human lung organoids have elucidated the infection strategies, it still is unknown how Pseudomonas adapt their behaviour during the infection process. First, they must be mobile to spread over the tissue surface, then quickly adhere to lung cells upon contact, and then activate their virulence factors. Despite the knowledge that bacteria can rapidly change their behaviour due to small signalling molecules, the technology to study these correlations was not available until now.
In Nature Communications, the researchers published their recent work to develop a biosensor to measure and track a small signalling molecule termed c-di-GMP in individual bacteria. Dr Jenal stated: “This is a technological breakthrough…Now we can monitor in real time and with high resolution how this signalling molecule is regulated during infection and how it controls the pathogen’s virulence. We now have a detailed view on when and where individual bacterial cells activate certain programs to regulate their behaviour. This method enables us to investigate lung infections in more detail.”
He concluded: “Thanks to the development of human lung organoids, we now have a much better understanding of how the pathogens behave in human tissue and presumably in patients. This brings us a big step closer to the goal of NCCR AntiResist.” Moving forwards, organ models will be imperative for developing new and effective strategies to combat pathogens.
The study relating to human lung organoids was published in Nature Microbiology.
Related topics
Antibiotics, Drug Discovery, Drug Targets, Organoids
Related conditions
Antimicrobial resistance (AMR), pneumonia
Related organisations
Biozentrum of the University of Basel
Related people
Dr Urs Jenal (Biozentrum of the University of Basel)