Elucidating the loss of mobility caused by LGMD2B
Posted: 27 June 2024 | Drug Target Review | No comments yet
The hiPSC-derived skeletal muscle model is the first to uncover the biological mechanisms underlying loss of mobility.
A novel approach to study rare muscle disorders named dysferlinopathy, or limb girdle muscular dystrophies 2B (LGMD2B), has been developed by biomedical engineers at Duke University. They grew complex, functional 3D muscle tissue from stem cells, which enabled the biological mechanisms underlying the loss of mobility caused by LGMD2B to be elucidated. Also, the team showed that a combination of existing treatments could alleviate certain symptoms of the disease.
LGMD2B, caused by a genetic disorder, prevents the production of the fully functional form of dysferlin protein, and affects around eight people per million globally. Dysferlin has many functions, such as sealing holes in muscle membranes, regulating calcium balances needed for muscle contraction and controlling cellular metabolism. The condition affects both men and women, presents later in life, and is rarely fatal, unlike Duchenne muscular dystrophy. Despite this, LGMD2B is extremely debilitating, with patients developing severe weakness in the legs and shoulders, which means they are required to use wheelchairs for the duration of their life. Presently, there are no approved treatments.
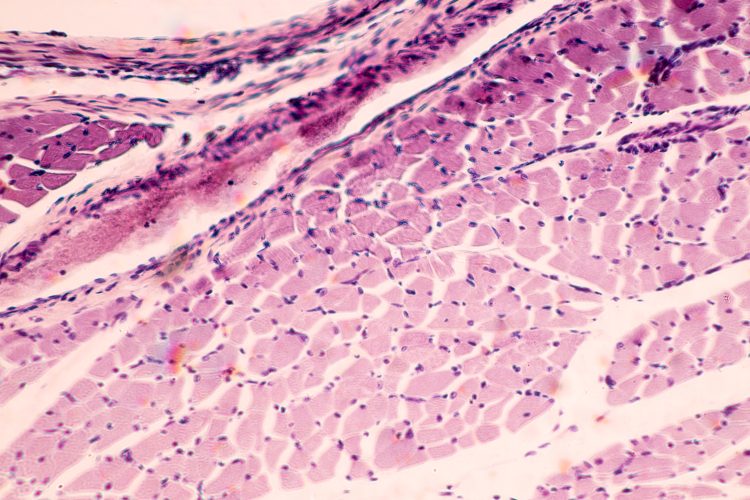
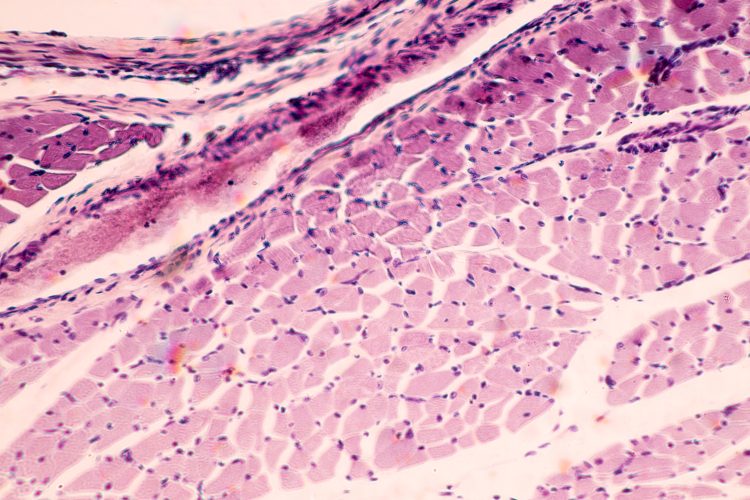
Furthermore, for unknown reasons, affected muscles accumulate fat within the muscle fibres themselves before degenerating and being replaced by fat cells. Dr Nenad Bursac, professor of biomedical engineering at Duke, stated: “This phenomenon is very rare even for muscular dystrophies…It’s a burning question within the community of why that happens.”
Significance of calcium
The Bursac Lab was the first to grow contracting, functional human skeletal muscle in a Petri dish and has been enhancing its processes ever since. In attempt to overcome the challenges associated with the study of LGMD2B, the research team worked on the engineered muscle platform for almost a decade.
Research into LGMD2B is very slow, as the mouse model used to replicate it presents very mild symptoms compared to human patients. The condition does not show until almost a year into the mice’s two-year long lifespan, and they can still walk. Additionally, dysferlin is expressed in various cell types, and blood levels of metabolic fuels like cholesterol are altered in mice and patients. As a result, it is challenging to evaluate the cell types responsible for the disease and whether metabolic changes are because of the loss of dysferlin itself or whole-body effects.
The scientists’ new system enabled them to focus singularly on the effects of dysferlin on skeletal muscle, minus the complications of other cell types or altered blood metabolite profiles. They started with induced pluripotent stem cells (iPSCs) derived from LGMD patients. Then, the stem cells were differentiated into muscle fibres, which exhibited numerous issues, like the muscles found in patients.
The findings were that the loss in muscle strength was due to the handling of calcium. Tests proved that the diseased muscle cells had leaks in their calcium reserves, meaning muscle contractions were weaker. Also, it was shown that the lack of dysferlin meant damage to the muscle cells went unrepaired, and that an inability to burn fatty acids was moderately to blame for the accumulation of fat within muscle fibres. Dr Khodabukus commented: “We replicated something seen in patients and showed that it’s not due to environmental factors within the body, but issues within the muscle itself.”
Dantrolene and vamorolone
Two drug candidates that have been identified through mouse models, but have not yet been tested in humans, were assessed: dantrolene, which prevents calcium from leaking from muscle cells’ reservoirs, and vamorolone, which was recently approved for use with Duchenne muscular dystrophy patients, but its mechanism is not fully understood. Used together, the drugs stopped the calcium leak aided cell membrane repair, restoring much of the muscles’ strength. However, although they also lessened the amount of fat accumulated within the muscles, they did not fully prevent it, or aid the muscles to burn fats efficiently.
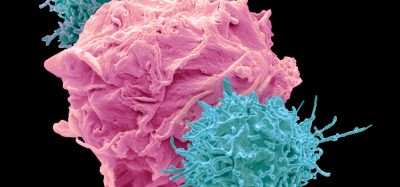
In the future, the team plan to add immune and fat cells to their experiments for greater complexity, which could ultimately lead to novel therapeutics that fully restore strength, repair and metabolic deficits. Dr Khodabukus concluded: “By building out our system more, we’ll hopefully be able to fully figure out what is driving the loss of muscle and its replacement by fat in these patients.”
This study was published in Advanced Science.
Related topics
Bioengineering, Drug Discovery Processes, Drug Targets, Induced Pluripotent Stem Cells (iPSCs), Organoids, Stem Cells, Targets
Related conditions
dysferlinopathy, limb girdle muscular dystrophies 2B (LGMD2B)
Related organisations
Duke University
Related people
Dr Nenad Bursac (Duke University)