DNA repair genes drive Huntington’s disease, UCLA study finds
Posted: 21 February 2025 | Drug Target Review | No comments yet
A new UCLA study reveals that DNA mismatch repair genes play a crucial role in Huntington’s disease by driving neuronal damage and motor impairments. Targeting these genes, especially Msh3 and Pms1, could offer promising therapeutic avenues for the disease.
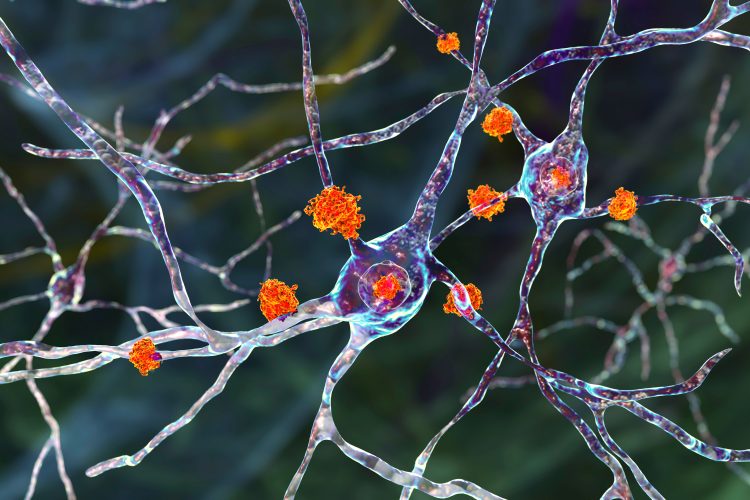
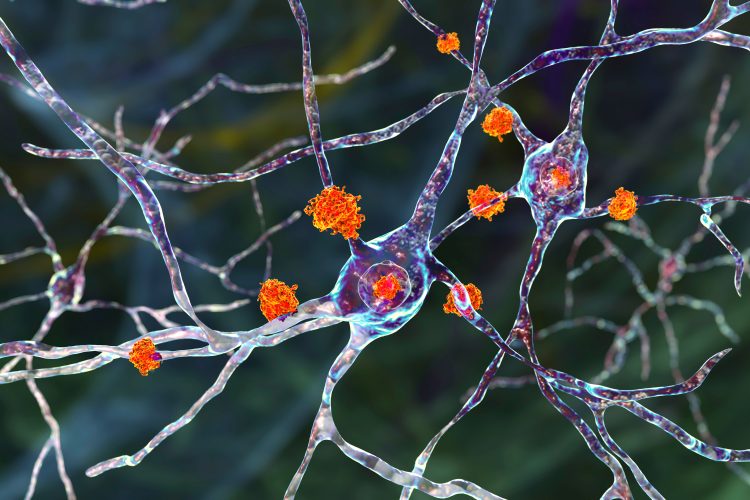
A new study from UCLA Health has revealed the crucial role of DNA repair genes in Huntington’s disease. By using mouse models, researchers found that genes involved in mismatch repair are key to the neuronal damage seen in the disease, triggering downstream pathologies and motor impairments. These findings uncover previously unknown mechanisms of the disease and suggest potential new directions for therapeutic development.
Understanding neuronal vulnerability in Huntington’s disease
One of the longstanding mysteries of Huntington’s disease, and indeed many other neurodegenerative conditions, is why the mutated huntingtin protein, present in every cell, selectively affects certain types of neurons. This new research offers a significant step towards understanding this phenomenon.
A recent human genetic study identified several DNA regions containing ‘modifiers’ for Huntington’s disease, which can influence the disease’s onset. Intriguingly, many of these regions contain genes involved in DNA mismatch repair. The UCLA study, published in the journal Cell, now reveals how a specific subset of these mismatch repair genes are key drivers of the disease and its impact on vulnerable neurons.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
“We demonstrate the same DNA mismatch repair genes that are modifiers in the Huntington’s disease patients can drive fast-paced disease processes only in the most vulnerable neurons in a mouse model, leading to a cascade of disease phenotypes,” said lead author Professor X. William Yang, a professor in the UCLA Health Department of Psychiatry and Biobehavioral Sciences and the Terry Semel Chair in Alzheimer’s Disease Research and Treatment at the Semel Institute.
Targeting mismatch repair genes
Yang and his team used mouse models with a high number of CAG repeats, necessary to observe disease features. They investigated whether genetically altering nine Huntington’s disease patient-derived modifier genes, including six mismatch repair genes, could influence disease characteristics. While the mouse model doesn’t exhibit overt neuronal cell death, it does display other crucial disease-like phenotypes, including gene expression dysregulation and the accumulation of mutant huntingtin protein aggregates, a hallmark of the disease.
Our study suggests that these genes are not just disease modifiers, as suggested by the previous studies, but are genetic drivers of Huntington’s disease.
The study found that mice lacking a subset of mismatch repair genes, particularly Msh3 and Pms1, showed a significant improvement in gene expression deficits and a reduction in mutant huntingtin aggregates. Furthermore, targeting Msh3 also led to improvements in locomotor and gait deficits, synaptic protein levels, and reduced glial cell over-reactivity.
“We were surprised to see the potent and sustained effects of targeting these mismatch repair genes in HD mice – the benefit lasts up to 20 months of age in a mouse, which would be comparable to about 60 years in humans,” said Yang. “Our study suggests that these genes are not just disease modifiers, as suggested by the previous studies, but are genetic drivers of Huntington’s disease.”
CAG repeat expansion
The research also sheds light on how mismatch repair genes influence the disease process. The team discovered that these genes drive a rapid rate of CAG repeat expansion in the most vulnerable neurons, and that this expansion is crucial for mutant huntingtin aggregation and gene expression dysregulation.
“These remarkable results demonstrate that a subset of mismatch repair genes is driving disease in vulnerable neurons because they confer the fastest rate of CAG repeat expansion in these neurons,” said Yang, “and our study provides mechanistic links that help to bridge modifier genes from patients, mismatch repair gene driven repeat expansion, and selective neuronal vulnerability in HD.”
Therapeutic implications and future directions
This study was published in Cell.
Related topics
Animal Models, Central Nervous System (CNS), Clinical Trials, Disease Research, Gene Therapy, Genomics, Neuroprotection
Related conditions
Huntington's disease
Related organisations
Semel Institute, UCLA Health
Related people
Professor X. William Yang