Bone repair breakthrough: why men and women heal differently
Posted: 24 April 2025 | Drug Target Review | No comments yet
Men and women heal bone injuries through distinct biological processes, challenging assumptions in regenerative medicine. The findings support the development of personalised implants and more effective, sex-specific treatment strategies.
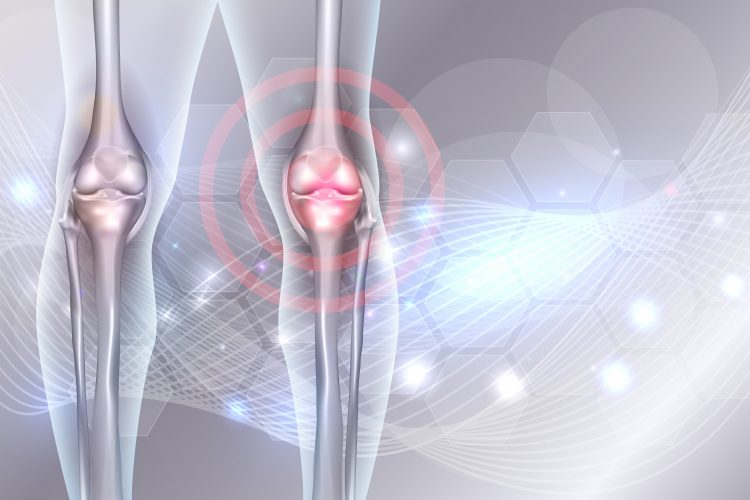
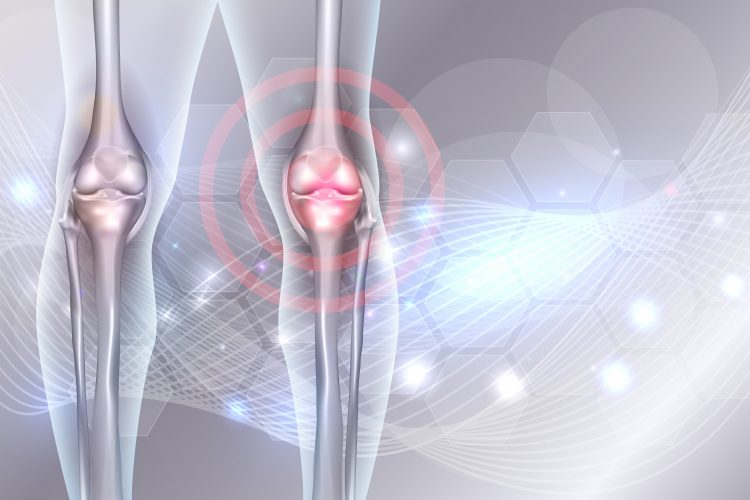
A new study, published in Bone Research, has revealed how biological sex and donor variability significantly influence bone healing, marking a major development for personalised medicine in tissue engineering.
Led by researchers at KU Leuven and collaborating institutions, the study highlights how different donor profiles lead to distinct healing mechanisms, offering promising solutions for tailoring bone implants and enhancing recovery from fractures.
Two healing roads: cartilage vs. fibrous pathways
Using innovative ‘callus organoids’ derived from human periosteal cells, scientists successfully modelled the critical cartilage-to-bone transition. They identified two distinct pathways: one involving hypertrophic cartilage (HyC) and the other fibrocartilage (FiC). These differences stemmed from early progenitor cell activation and were closely linked to the donor’s biological sex.
Organoids from male donors formed larger, cartilage-rich structures with high levels of glycosaminoglycans and collagen II – key markers of hypertrophic cartilage. Female-derived organoids, on the other hand, produced denser, fibrous tissue lacking these classic features. Despite the structural divergence, both tissue types successfully matured into bone when implanted in mice.
Shared secret for success: a common protein panel
Central to both healing pathways was a shared set of 84 secreted proteins absent in non-regenerating tissues. Key players included AGRIN, SPP1 (osteopontin), ANGPL4, NPP2 (autotaxin), and BMP1, proteins known for driving matrix remodelling, bone maturation, and vascular development.
These molecules could become key tools for noninvasively tracking bone healing, enhancing implant quality checks and post-surgery monitoring.
Biological sex shapes regeneration capacity
One of the study’s most striking findings was the sex-dependent nature of progenitor cell behaviour. Male-derived cells showed faster proliferation and produced more extracellular matrix, ultimately resulting in larger regenerated bone volumes. Female-derived cells, while forming denser tissues, followed a different but equally effective path to bone formation.
By decoding sex-specific repair mechanisms, we can design smarter living implants tailored to individual but also groups of patients.
“Our work bridges the gap between developmental biology and clinical translation. By decoding sex-specific repair mechanisms, we can design smarter living implants tailored to individual but also groups of patients.” said Professor Ioannis Papantoniou, senior author of the study. “The secreted protein panel is a game-changer for monitoring implant quality without invasive sampling.”
Clinical impact: toward personalised bone repair
These insights arrive at a critical time in regenerative medicine. Bone regeneration remains an unpredictable process, particularly for younger patients (aged 25–45) suffering from non-union fractures. Traditional approaches overlook donor-specific and sex-related factors, limiting the efficacy of existing treatments.
This study not only brings clarity to the cartilage-to-bone transition but also introduces a powerful set of biomarkers for predicting therapeutic outcomes, streamlining implant manufacturing and reducing clinical risk.
What’s next: hormones, models, and translation
The next steps in this research include validating these protein markers in larger animal models and investigating the influence of hormonal environments on regeneration. These efforts aim to refine the approach further, ultimately enabling clinicians to select the best therapeutic strategies based on individual biological profiles.
This study redefines fracture healing and establishes a new foundation for personalised tissue engineering, where sex, biology, and precision science shape the future of bone repair.
Related topics
Biomarkers, Cell Regeneration, Cell Therapy, Organoids, Personalised Medicine, Regenerative Medicine, Translational Science
Related conditions
bone fractures
Related organisations
KU Leuven
Related people
Professor Ioannis Papantoniou