New genetic analysis reveals early diagnosis for breast cancer
Posted: 15 August 2017 | Dr Zara Kassam (Drug Target Review) | No comments yet
Researchers have shown that catching and treating breast cancer before it spreads is now a realistic goal…
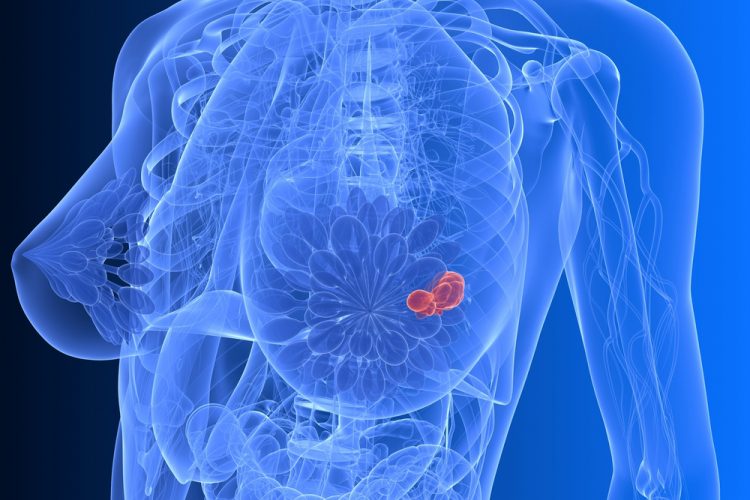
Researchers have shown that catching and treating breast cancer before it spreads is now a realistic goal, It also opens the door to predicting which drugs will work against breast cancer that has already spread.
Scientists have investigated how breast cancer evolves from an original tumour in the breast to tumours that have spread, or metastasised, this shows promise for breast cancer patients as diagnosing and treating the breast cancer at early stages means there is a greater chance of preventing cancer cells spreading to other tissues, such as the lungs, brain and bone. The research was published in Cancer Cell,
“As the cells that cause the spread of breast cancer leave relatively late, it means they are still quite similar to the cells in the primary tumour. Therefore, by studying the genome of the primary breast cancer tumour, in the future we may be able to predict what cells that might have spread ‘look’ like, and potentially which treatments they will respond to,” said Dr Lucy Yates, first author from the Wellcome Trust Sanger Institute and Guys and St Thomas’ NHS Trust.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
The research team found that most of the genetic changes in the original breast tumour were also present in the metastatic tumours, showing that the cancer cells spread late in disease development.
In the retrospective study, the team sequenced the DNA of 299 tumours from 170 patients with breast cancer that either returned in the remaining breast – local relapse – or had spread – metastatic breast cancer.
Researchers found that in the time between breast cancer patients being diagnosed with primary cancer and the diagnosis of metastasis, the breast cancer cells had gained genetic changes, or mutations, that increased the aggressiveness of the tumour. This may explain why metastatic breast cancer is currently difficult to treat.
“Most women who have metastatic breast cancer do not have another biopsy of the cancer, and rarely have it analysed using genetic sequencing. In this study, we found that in some cases, the metastatic tumours had particular genetic changes that could be targeted with treatments. We would not have seen these mutations by sequencing the primary tumour alone. Our results suggest that it should be more routine to biopsy the metastasis and have it genetically analysed in order to open up clinical trials of treatment options for metastatic breast cancer,” said Professor Per Eystein Lønning, the joint lead author from the University of Bergen and Haukeland University Hospital in Bergen.
Studies are now open to recruiting patients with metastatic breast cancer across Europe – these studies will first extend the analysis performed here to many more patients, but the ultimate goal is to build a platform for identifying an appropriate clinical trial of new treatments for each patient with metastatic breast cancer.
The use of whole-genome sequencing enables researchers to accurately distinguish between tumour types with different treatment strategies. In one particular case, it was thought a patient had primary breast cancer that had relapsed in the breast. However, after sequencing the tumour, the team found it was not a relapse but a second primary breast cancer. Genomic data enabled the scientists to tell these two scenarios apart, which would have changed the treatment philosophy used – this would be difficult using standard diagnostic methods.
“Our study shows that in order to catch breast cancer before it spreads, early detection of breast cancer is key, and we provide a good rationale for continuing to improve methods for detecting breast cancer sooner. These results show the power of genetic sequencing in understanding metastatic breast cancer and open the door to personalised treatment for breast cancer in the future,” said Dr Peter Campbell, joint lead author and head of the Cancer, Ageing and Somatic Mutation Programme at the Wellcome Trust Sanger Institute
Related topics
Drug Targets, Genetic Analysis, Genomics, Oncology
Related conditions
Breast cancer
Related organisations
Guys and St Thomas’ NHS Trust, Haukeland University Hospital in Bergen, University of Bergen, Wellcome Trust Sanger Institute
Related people
Dr Lucy Yates, Professor Per Eystein Lønning