Researchers create anti-inflammatory antibodies to treat autoimmune disease
Posted: 22 December 2017 | Steve Bremer (Drug Target Review) | No comments yet
Massachusetts General Hospital (MGH) investigators use enzyme treatment to convert autoantibodies into anti-inflammatory antibodies in animal models of two autoimmune diseases.
Researchers have engineered antibodies within an organism, converting autoantibodies that attack ‘self’ tissues into anti-inflammatory antibodies in animal models of two autoimmune diseases.
“We were able to convert antibodies that cause autoimmune disease into anti-inflammatory antibodies by specifically modifying the sugars attached to the antibodies,” said Robert Anthony, from the MGH Division of Rheumatology, Allergy and Immunology, who led the study. “While more work is required, we hope that this approach of anti-inflammatory antibody conversion will have a beneficial effect on patients suffering from autoimmune and inflammatory diseases.” The study will be published in the January 25 issue of Cell and has been released online.
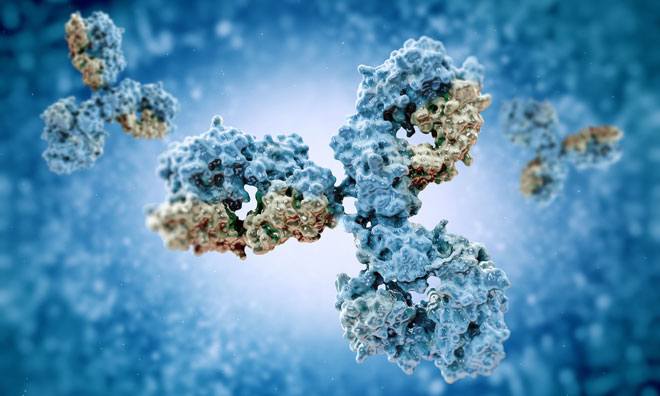
Intravenous immunoglobulin (IVIG) – prepared from the antibodies of healthy donors – is used at low doses to treat patients lacking key antibodies. Paradoxically, at high dosage levels IVIG can suppress, rather than enhance the immune response and is used to treat several inflammatory and autoimmune conditions. Whether activated antibodies stimulate an inflammatory or anti-inflammatory response appears to be determined by specific sugar molecules called glycans attached to the Fc region – the tail-like section of a Y-shaped antibody. In previous work, Anthony’s group and others have found that the anti-inflammatory effect of high-dose IVIG can be attributed to a minor fraction of antibodies to which a glycan called sialic acid has been attached to their Fc region.
While glycans are usually attached to the proteins making up antibodies while they are being assembled within cells, recent evidence suggests they could be modified outside of the cellular environment. The MGH team set out to determine whether administration of a transferase, an enzyme that moves chemical groups like glycans from one molecule to another, could convert inflammatory antibodies to anti-inflammatory forms within a living animal.
Since the attachment of sialic acid to an Fc group requires the presence of another glycan called galactose, the team created two enzymes termed B4Fc and ST6Fc, which induce the attachment of galactose and sialic acid respectively. Although intravenous administration of either enzyme alone did not reduce inflammation in a mouse model of rheumatoid arthritis, simultaneous administration of both in a form called B4ST6Fc had anti-inflammatory effects similar to those of high-dose IVIG. B4ST6Fc administration also reduced kidney damage in a mouse model of lupus-related kidney inflammation.
Additional experiments found little evidence that enzyme administration affected antibodies not involved with the specific autoimmune condition and also showed that platelets, which become activated at the site of antibody-driven inflammation, provided the sialic acid and galactose attached to the Fc region by the B4ST6Fc enzyme.
Anthony explains that, while IVIG can be effective against many inflammatory and autoimmune diseases, it is in short supply, the treatment is expensive, and administration is time consuming. “We found that our enzymes were effective at a 400-fold lower dose than high-dose IVIG, and by manipulating the enzymes already in an organism, our method eliminates the need for a lengthy IVIG infusion.” His team will be exploring questions in future studies such as appropriate dosage, optimal administration and whether repeat treatments would be required.
Related topics
Antibodies, Immunology
Related conditions
Lupus, rheumatoid arthritis
Related organisations
Massachusetts General Hospital
Related people
Robert Anthony