Detecting prostate tumour cells in blood can give an early warning of treatment failure
Posted: 23 March 2015 | Victoria White
A blood test that measures the number of prostate tumour cells shed into the bloodstream can act as an early warning sign that treatment is not working…
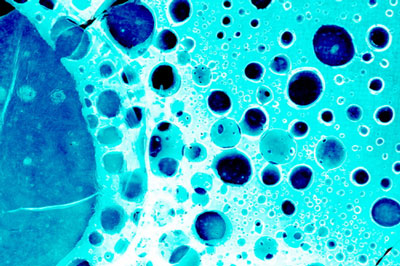
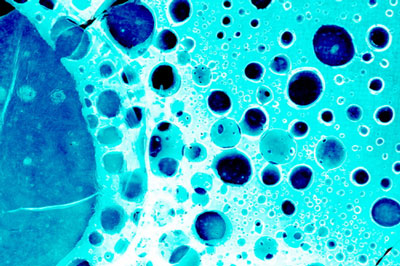
A blood test that measures the number of cells shed from prostate tumours into the bloodstream can act as an early warning sign that treatment is not working, a major new study shows.
Researchers showed that measuring the numbers of circulating prostate tumour cells in the blood predicted which men were benefitting least from a prostate cancer drug after as little as 12 weeks of treatment.
They hope their work will allow doctors to switch patients to alternative treatments earlier than is currently possible, if these results are confirmed by further studies. The research could also hasten the development of cancer treatments by speeding up clinical trials, since doctors could tell much earlier whether a treatment is working.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
The study was led in the UK by researchers at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, and also involved several leading international institutions.
It was funded by a range of organisations including a Medical Research Council biomarkers grant, the companies Janssen Diagnostics, the Prostate Cancer Foundation in the US, and Prostate Cancer UK.
As tumours grow and progress, they shed cancer cells into the bloodstream, some of which can seed new secondary tumours elsewhere in the body. So the researchers wanted to see whether a high number of circulating prostate tumours cells was an indication of a growing tumour that wasn’t responding to treatment, and could predict a lower chance of survival.
The study, published in the Journal of Clinical Oncology, involved the detailed analysis of blood samples from 711 men who took part in a major phase III trial of the prostate cancer drug abiraterone.
Researchers measured numbers of circulating prostate tumour cells at four-week periods after the start of treatment with the drug, along with a range of other biomarker molecules in the blood including lactate dehydrogenase (LDH), high levels of which are a sign of general tissue damage.
The trial itself had used the standard trial end points of average overall survival and survival free of cancer progression to show abiraterone’s effectiveness in late-stage prostate cancer. But the researchers were able to cross-reference those results with data on circulating tumour cells and LDH levels in each man taking part.
They found a correlation between those men who had responded least well to treatment with abiraterone, and higher levels of cancer cells and LDH in the bloodstream, measured 12 weeks after starting treatment. They showed that levels of circulating tumour cells varied independently of a range of other biomarkers.
To prove the effectiveness of a new drug, clinical trials normally need to be run until the cancer is progressing clinically for each patient – and often until many of the patients on the trial have died. But with this new blood test, it might be possible to use circulating tumour cells as an early indicator that a drug is or is not working, and as a predictor of survival.
Circulating prostate tumour cells act as early warning test for treatment response
Study leader Professor Johann de Bono, Professor of Experimental Cancer Therapeutics at The Institute of Cancer Research, London, and Honorary Consultant at The Royal Marsden NHS Foundation Trust, said: “The past decade has seen unprecedented success in the development of new drugs for advanced, metastatic prostate cancer. One of the major challenges we face now is in optimising the use of these new treatments by making sure that the right men receive them, and only for as long as they are benefitting.
“Our study showed that circulating tumour cells act as an early warning test for men who are not responding to treatment – potentially allowing doctors to switch patients early to alternative options. We hope our results will not only lead to better use of the current range of treatments, but also speed up the discovery of new drugs by providing an important new tool to the researchers trialling them.”
Professor Paul Workman, Chief Executive of The Institute of Cancer Research, London, said: “Using a blood test to assess whether a cancer drug is working would be much easier and more convenient than other methods of monitoring treatment, and might pick up signs that a tumour is not responding weeks or months earlier than is achievable now. It could give doctors a valuable early warning that treatment is not working, and an opportunity to switch the patient promptly to an alternative drug.”
Related topics
Biomarkers
Related organisations
Cancer Research, The Institute of Cancer Research (ICR)