Stem cell therapy discovery for age-related macular degeneration
Posted: 3 January 2018 | Dr Zara Kassam (Drug Target Review) | No comments yet
Stem cell-derived retinal cells need primary cilia to support the survival of light-sensing photoreceptors…


Scientists at the National Eye Institute (NEI), part of the National Institutes of Health, report that tiny tube-like protrusions called primary cilia on cells of the retinal pigment epithelium (RPE) — a layer of cells in the back of the eye — are essential for the survival of the retina’s light-sensing photoreceptors.
The discovery has advanced efforts to make stem cell-derived RPE for transplantation into patients with geographic atrophy, otherwise known as dry age-related macular degeneration (AMD), a leading cause of blindness.
“We now have a better idea about how to generate and replace RPE cells, which appear to be among the first type of cells to stop working properly in AMD,” said the study’s lead investigator, Dr Kapil Bharti, Stadtman investigator at the NEI. Dr Bharti is leading the development of patient stem cell-derived RPE for an AMD clinical trial set to launch in 2018.
In a healthy eye, RPE cells nourish and support photoreceptors, the cells that convert light into electrical signals that travel to the brain via the optic nerve. RPE cells form a layer just behind the photoreceptors. In geographic atrophy, RPE cells die, which causes photoreceptors to degenerate, leading to vision loss.
Dr Bharti and his colleagues are hoping to halt and reverse the progression of geographic atrophy by replacing diseased RPE with lab-made RPE. The approach involves using a patient’s blood cells to generate induced-pluripotent stem cells (iPSCs), cells capable of becoming any type of cell in the body. iPSCs are grown in the laboratory and then coaxed into becoming RPE for surgical implantation.
Attempts to create functional RPE implants, however, have hit a recurring obstacle: iPSCs programmed to become RPE cells have a tendency to get developmentally stuck, said Dr Bharti. “The cells frequently fail to mature into functional RPE capable of supporting photoreceptors. In cases where they do mature, however, RPE maturation coincides with the emergence of primary cilia on the iPSC-RPE cells.”
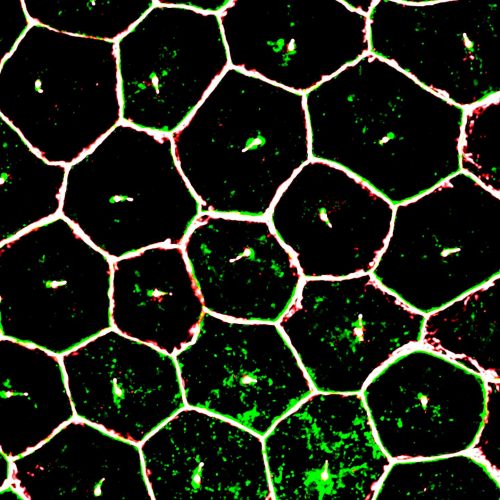
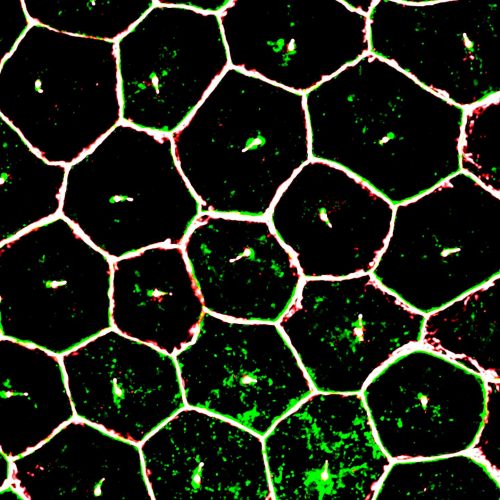
Mature iPSC-derived RPE cells are visible by super-resolution confocal microscopy. One primary cilium resides in the centre of each cell. RPE cell borders are stained showing tight junction markers. Credit -Dr Ruchi Sharma, NEI.
The researchers tested three drugs known to modulate the growth of primary cilia on iPSC-derived RPE. As predicted, the two drugs known to enhance cilia growth significantly improved the structural and functional maturation of the iPSC-derived RPE. One important characteristic of maturity observed was that the RPE cells all oriented properly, correctly forming a single, functional monolayer. The iPSC-derived RPE cell gene expression profile also resembled that of adult RPE cells. And importantly, the cells performed a crucial function of mature RPE cells: they engulfed the tips of photoreceptor outer segments, a pruning process that keeps photoreceptors working properly.
By contrast, iPSC-derived RPE cells exposed to the third drug, an inhibitor of cilia growth, demonstrated severely disrupted structure and functionality.
As further confirmation of their observations, when the researchers genetically knocked down expression of cilia protein IFT88, the iPSC-derived RPE showed severe maturation and functional defects, as confirmed by gene expression analysis. Tissue staining showed that knocking down IFT88 led to reduced iPSC-derived RPE cell density and functional polarity, i.e., cells within the RPE tissue pointed in the wrong direction.
Dr Bharti and his group found similar results in iPSC-derived lung cells, another type of epithelial cell with primary cilia. When iPSC-derived lung cells were exposed to drugs that enhance cilia growth, immunostaining confirmed that the cells looked structurally mature.
The report suggests that primary cilia regulate the suppression of the canonical WNT pathway, a cell signalling pathway involved in embryonic development. Suppression of the WNT pathway during RPE development instructs the cells to stop dividing and to begin differentiating into adult RPE, according to the researchers.
The researchers also generated iPSC-derived RPE from a patient with ciliopathy, a disorder that causes severe vision loss due to photoreceptor degeneration. The patient’s ciliopathy was associated with mutations in cilia gene CEP290. Compared to a healthy donor, iPSC-derived RPE from the ciliopathy patient had cilia that were smaller. The patient’s iPSC-derived RPE also had maturation and functional defects similar to those with an IFT88 knockdown.
Further studies in a mouse model of ciliopathy confirmed an important temporal relationship: Looking across several early development stages, the RPE defects preceded the photoreceptor degeneration, which provides additional insights into ciliopathy-induced retinal degeneration.
The study’s findings have been incorporated into the group’s protocol for making clinical-grade iPSC-derived RPE. They will also inform the development of disease models for research of AMD and other degenerative retinal diseases, Dr Bharti said.
The study appears in Cell Reports.
Related topics
Clinical Trials, Microscopy, Stem Cells
Related conditions
age-related macular degeneration (AMD)
Related organisations
National Eye Institute, National Institutes of Health (NIH)
Related people
Dr Kapil Bharti