Researchers use AI technology to chart immune cell receptor
Posted: 10 January 2018 | Drug Target Review | No comments yet
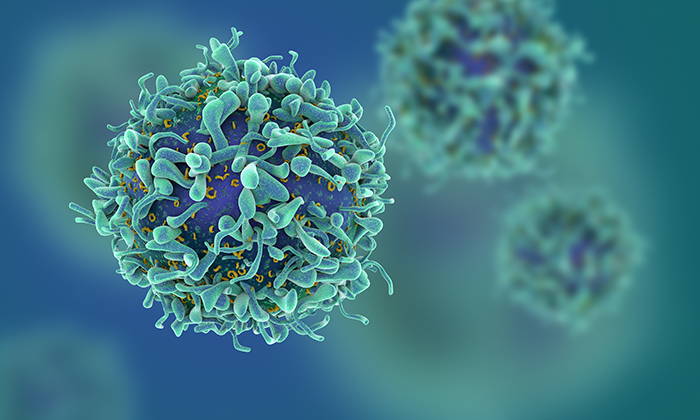
Johns Hopkins scientists have used a form of artificial intelligence to create a map that compares types of cellular receptors, the chemical ‘antennas’ on the surface of immune system T-cells.
Their experiments with lab-grown mouse and human T-cells suggest that people with cancer who have a greater variety of such receptors may respond better to immunotherapy drugs and vaccines.
A report on how the scientists created and tested what they call ‘ImmunoMap’ appeared in Cancer Immunology Research.
“ImmunoMap gives scientists a picture of the wide diversity of the immune system’s responses to cellular antigens,” says Jonathan Schneck, M.D., Ph.D., professor of pathology, medicine and oncology at the Johns Hopkins University School of Medicine, and a member of the Johns Hopkins Kimmel Cancer Center.
Receptors on T-cells recognise antigens, or pieces of other cells that trigger an immune response, particularly antibodies. If the antigens are foreign, T-cells raise the alarm within the immune system, which can distribute an ‘all-points bulletin’ to be on the lookout for the unfamiliar antigens.
Because diseases such as cancer tend to evade detection by T-cells’ receptors, allowing a tumour to grow unchecked, scientists have long sought ‘intel’ on this process as a means of developing therapies that target malignant cells, but leave healthy cells alone.
“Much of immunotherapy today is built on the premise that we know these antigens,” says Johns Hopkins biomedical engineering M.D./Ph.D. student John-William Sidhom. “But we actually don’t know as much as we need to about them and the T-cells that recognise them.”
To address that need, Sidhom used high-powered computing to create a mathematical model–essentially a digital map–of genomic sequence data of receptors from human T-cells that were exposed to a virus in the laboratory. “Our goal was to cluster T-cell receptors that are similar and may target the same antigen,” says Sidhom.
Using an unsupervised learning algorithm, the team was able to convert the T-cell receptor sequencing data into numeric distances based on similarities in the receptor sequences and cluster them by functional specificity. For example, if two receptor sequences were similar, the computer assigned a short distance rank between the two sequences. If the sequences were different, they received a longer distance rank.
Once the thousands of sequences were converted into these ‘distance’ metrics, the computer system’s artificial intelligence algorithms looked for patterns among the receptors.
“That’s how we got ImmunoMap, by characterising receptor sequences as they relate to each other,” says Schneck. “T-cell receptors that are very similar, with slight differences in their sequences, may be recognising the same antigen.”
The Johns Hopkins team tested ImmunoMap’s ability to correlate immune responses on receptor sequencing data from T-cells in the tumours of 34 patients with cancer enrolled in a nationwide clinical trial of the immunotherapy drug nivolumab.
Of the 34, three patients with melanoma responded to nivolumab, and the rest did not respond. In the responders, the scientists found more–an average of 15–different T-cell receptor clusters compared with eight to nine in the non-responders.
The scientists also found that the diversity of T-cell receptors decreased among the responders by 10-15% four weeks after nivolumab treatment.
“Those patients had a broad array of receptor weaponry before their treatment, which may have allowed the right receptor to kill their cancer cells,” says Schneck. “Once their immune system found the correct receptor, T-cells expressing those receptors multiplied, leading to an overall reduction in the structural diversity of their T-cell receptors.”
Schneck says some scientists have emphasized that response to immunotherapy is largely dependent on whether T-cells are infiltrating the tumour site, but his research suggests that while, “infiltration is important, it’s not enough to explain patients’ variable responses to immunotherapy drugs.”
The team also created an ImmunoMap of the diversity of T-cell receptors specific for tumour antigens in mice with and without tumours. Their analysis showed that the diversity of T-cell receptors decreased among samples of T-cells taken closer to the tumour, compared with farther away. The data may help scientists determine how tumours evade detection by the immune system.
Schneck says the research group also needs to amass more ImmunoMap data to reliably predict which patients may or may not respond to immunotherapy. “At this point, ImmunoMap can’t match T-cell receptors to specific antigens, or determine whether those antigens are important for immunotherapy response in any individual patient,” he notes.
But the hope, he says, is that ImmunoMap may one day be helpful in designing vaccines and engineered T-cells for cancer treatment.
Related topics
Artificial Intelligence, Immuno-oncology, Immunotherapy, T cells
Related conditions
Cancer
Related organisations
John Hopkins University
Related people
John-William Sidhom, Jonathan Schneck