Next-generation therapeutic helps immune cells detect, destroy cancer
Posted: 4 July 2018 | Drug Target Review | No comments yet
Researchers have found that cancer cells evade destruction by macrophages in two ways…
Macrophages – immune cells that engulf and digest particles and pathogens – provide the first line of defence against bacteria and viruses and can also help destroy cancer cells. Macrophages play a paradoxical role, with M1 macrophages rousing the immune system to activate and M2 macrophages quelling inflammation. Researchers have found that cancer cells evade destruction by macrophages in two ways – by converting cells to become docile, M2 macrophages, and by sending out a signal that tricks M1 macrophages into letting them be. Investigators from Brigham and Women’s Hospital have developed a therapeutic that delivers a double whammy to knock out both mechanisms. In preclinical models, the new approach has yielded promising results.
“Clinicians are increasingly realising that one drug or a one-size-fits-all approach is not enough when combatting cancer and that a combination immunotherapy, such as blocking two distinct targets in the same immune cell, is the future of immuno-oncology. Our approach capitalises on this concept,” said co-corresponding author Dr Ashish Kulkarni, a former instructor in the Division of Engineering in Medicine at BWH and assistant professor in the Department of Chemical Engineering at the University of Massachusetts, Amherst.
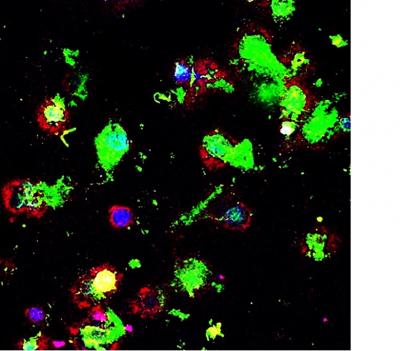
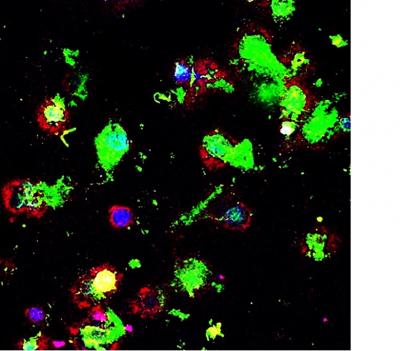
Confocal microscopy image shows macrophages (red) engulfing cancer cells (green). Ashish Kulkarni, Brigham and Women’s Hospital
Dr Kulkarni and colleagues have previously reported on the design and engineering of supramolecules – therapeutics that are built from component molecules that click together like building blocks. To reinvigorate macrophages, the team designed a supramolecule that could block the “don’t eat me” signal that cancer cells can produce and simultaneously inhibit signalling that converts macrophages to M2 subtype.
The researchers tested the supramolecular therapeutic in animal models of aggressive forms of breast cancer and skin cancer, comparing their drug directly with a drug currently available in the clinic. Mice that were untreated formed large tumours by Day 10. Mice treated with currently available therapies showed decreased tumour growth. But mice treated with the new supramolecular therapy had complete inhibition of tumour growth. The team also reported an increase in survival and a significant reduction in metastatic nodes.
“We can actually see macrophages eating cancer cells,” said co-corresponding author Dr Shiladitya Sengupta, BWH associate bioengineer and assistant professor of medicine at Harvard Medical School, citing confocal microscopy images published in the paper that show macrophages (red) engulfing cancer cells (green).
The researchers plan to continue testing the new therapy in preclinical models to evaluate safety, efficacy and dosage. The supramolecular therapy they have designed has been licensed and they hope to move the therapeutic into clinical trials in the years ahead should preclinical testing continue to show promise.
The team’s findings are published today in Nature Biomedical Engineering.
Related topics
Drug Targets, Immuno-oncology, Immuno-oncology therapeutics, Immunology, Oncology, Therapeutics
Related conditions
Cancer
Related organisations
Brigham and Women's Hospital, Massachusetts University
Related people
Dr Ashish Kulkarni








