New drugs targeting gut microbes may reduce the risk of cardiovascular disease
Posted: 7 August 2018 | Drug Target Review | No comments yet
The new class of drugs are mechanism-based inhibitors which potentially interrupt the gut microbial pathway that produces TMAO…
Researchers have designed a new class of drugs which target a specific microbe pathway in the gut, which may reduce the risk of cardiovascular disease.
The non-antibiotic compounds were tested in animal models and prevented the production of a by product in the gut which is linked to strokes and heart attacks in humans.
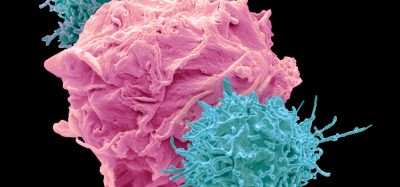
In contrast to antibiotics, which non-specifically kill bacteria, the team from Cleveland Clinic designed the compounds to prevent gut microbes from making a harmful molecule, without killing the microbes, as these are part of gut flora and may be beneficial to overall health of an individual.
The in vivo experiments in mice saw the drugs reverse two major risk factors for cardiovascular disease; excessive clot formation and increased platelet responsiveness. The drugs lowered levels of a gut bacteria by-product, trimethylamine N-oxide (TMAO), which forms during digestion.
Dr Stanley Hazen led the researcher and previously found that high levels of TMAO in the blood as being a powerful method of predicting future risks of stroke, heart attack and cardiovascular related death.
The new class of drugs are mechanism-based inhibitors which potentially interrupt the gut microbial pathway that produces TMAO. These compounds are structurally similar to choline, bacterial cells are ‘tricked’ into taking them up as nutrients, and once inside the microbe, the inhibitors are then able to block the production of TMAO by inactivating choline utilisation protein C (cutC), a gut microbe enzyme.
“To our knowledge, this is the most potent therapy to date for ‘drugging’ the microbiome to alter a disease process. In addition, gut bacteria are altered but not killed by this drug, and there were no observable toxic side effects,” said Dr Hazen.
“The approach developed could potentially be used to target other gut microbial pathways. We look forward to advancing this novel therapeutic strategy into humans.”
The researchers identified that in animal models a single oral dose of a potent inhibitor significantly reduced levels of TMAO in blood for up to three days. The inhibitor also reversed heightened thrombus formation and enhanced platelet responsiveness after arterial injury.
In the animal models the drug mostly stayed in the gut targeting the microbial pathway and was minimally absorbed by the body. The team also identified that the drugs reduced ‘hyper-responsive’ platelet function to a normal level, which inhibited excessive blood clot formation. The models showed little risk of bleeding – a common side effect of other anti-platelet therapies.
Since the drugs were designed not to kill bacteria, it is likely they will not contribute to antibiotic resistance.
The study was published in Nature Medicine.
Related topics
Disease Research, Drug Delivery, Drug Discovery, Drug Targets, Research & Development
Related conditions
Cardiovascular disease, Heart attack, Stroke
Related organisations
Cleveland Clinic
Related people
Dr Stanley Hazen