Halting the spread of brain cancer
Posted: 26 November 2018 | Drug Target Review | No comments yet
Mouse models used to show how convection enhanced delivery caused glioma cells to invade the rest of the brain could help to prevent this spread in future…
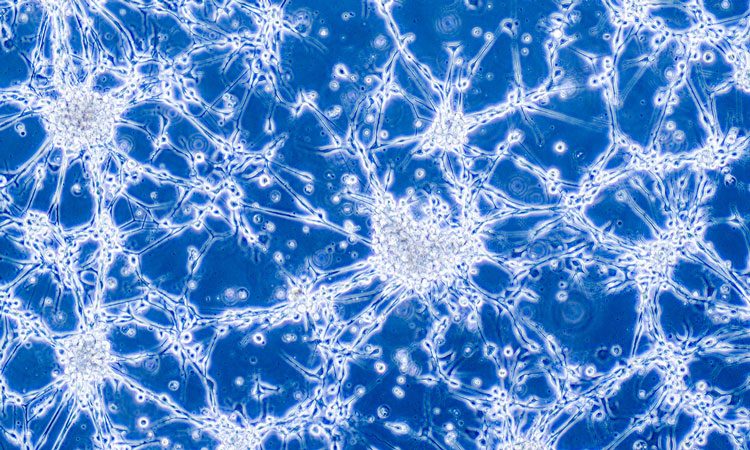
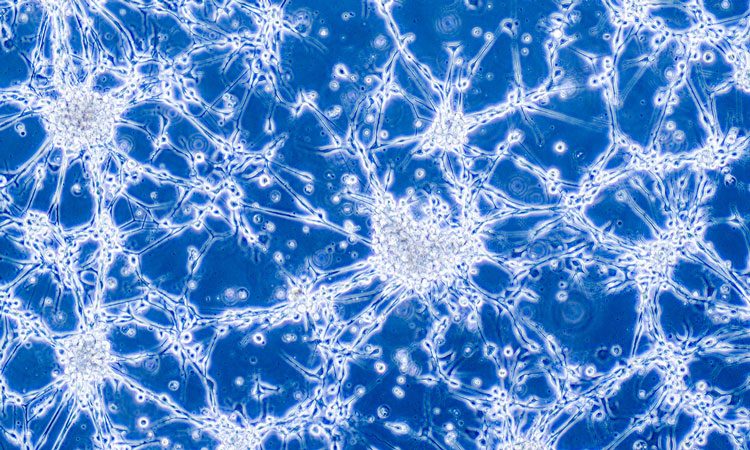
The tissues in our bodies are largely made of fluid that moves around cells and is essential to normal bodily function. In some cases, this fluid may be doing more harm than good.
In people who have glioblastoma, the deadliest form of brain cancer, this fluid has a much higher pressure, causing it to move fast, forcing the cancer cells to spread. And a common cancer therapy, which inserts a drug directly into the tumor with a catheter, can make this fluid move even faster.
A team of researchers at Virginia Tech, led by Dr Jennifer Munson, an Assistant Professor in the Department of Biomedical Engineering and Mechanics in the College of Engineering, may have found a solution to stopping this inevitable cancer cell spread.
Dr Chase Cornelison, lead author and a postdoctoral researcher at Virginia Tech, details the use of a drug that Prof Munson’s team found can block the way cancer cells respond to fluid flow. This work is part of a five-year research grant project across multiple universities, examining the role of interstitial fluid flow in the spread of glioma cells. Interstitial fluid is the fluid that surrounds cells in the body.
In labs, Dr Cornelison and others on Munson’s team used mice with glioblastoma to test how a particular approach to delivering cancer treatment, called convection enhanced delivery, caused glioma cells to invade the rest of the brain. To block the fluid’s rapid movement and the spread of cancer cells, they tested a drug called AMD3100. The drug, which already has been used in clinics, appeared to be a game changer, Dr Cornelison said.
The majority of this research happened at the University of Virginia, where Prof Munson previously worked before she came to Virginia Tech in 2017.
This finding could lead to stopping glioblastoma from spreading, Dr Cornelison said.
“I am hopeful that since the drug that we used to block flow stimulation is currently used in patients that maybe clinicians, when they do consider using convection enhanced delivery, will combine that with this drug,” he said.
Prof Munson has been studying glioblastoma for more than 10 years, with a more recent focus on the role of interstitial fluid flow on cancer cells and the brain.
“It [glioblastoma] is so deadly, and there hasn’t been a shift in treatment response in decades. Something needs to change,” she said. “With my expertise and looking at fluid flow, maybe there’s an answer there that we haven’t seen.”
Raising awareness of interstitial fluid flow throughout the body is Prof Munson’s aim in her research.
“This is a force that isn’t accounted for much in brain tissues,” she said. “My goal is to have more people thinking about this force and that it can actually have effects on cells that we don’t intend.”
The article was published in Scientific Reports.
Related topics
Analytical Techniques, Disease Research, Drug Discovery, Drug Targets, In Vivo, Oncology, Research & Development
Related conditions
Glioblastoma
Related organisations
Virginia University
Related people
Dr Chase Cornelison, Professor Jennifer Munson