FGL2 protein may be an effective target for GBM
Posted: 28 January 2019 | Drug Target Review | No comments yet
Researchers have discovered an immune regulator that appears to dictate glioblastoma progression by shutting down immune surveillance…
Researchers have discovered an immune regulator that appears to dictate glioblastoma (GBM) progression by shutting down immune surveillance, indicating a potential new area of therapeutic investigation.
“Classical wisdom is that brain tumour progression is linked to oncogene activation and tumour suppressor gene inactivation; however genetic and epigenetic mutations are not the only cause of GBM progression,” said Shulin Li, Ph.D., professor of Pediatrics. “Some immune regulators can do the same thing and are key regulators of cancer, especially in certain tissues and environmental contexts.”
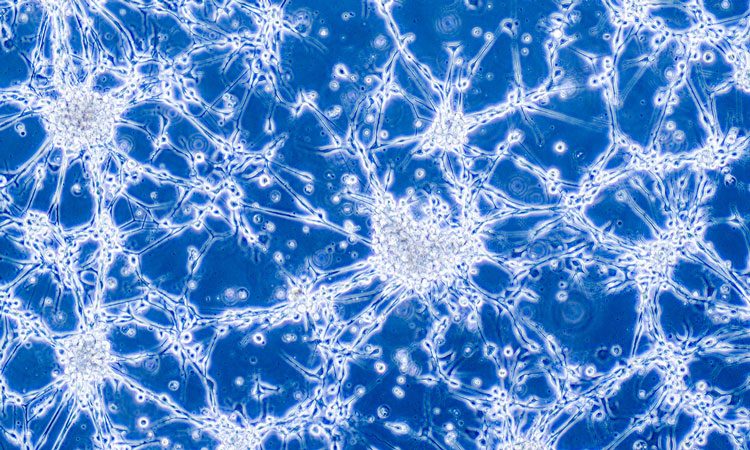
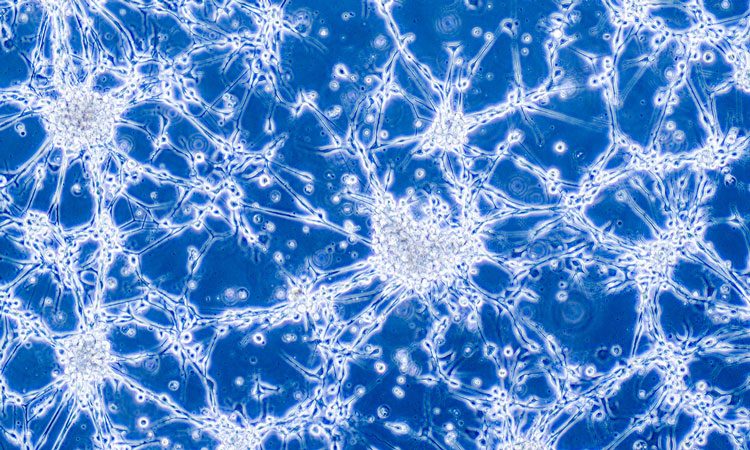
GBM, unlike melanoma and lung cancers, does not attract robust T-cell immune responses, and, so far, immunotherapies have had little success against it. GBM is considered “immunologically cold” or unreactive likely due to a tumour elaborated immune suppressive factors.
Findings from the study indicate FGL2 (fibrinogen-like protein 2), which is known for suppressing the immune system, is highly expressed in GBM. Investigators showed that inactivating or “knocking out” FGL2 from the tumour cells can eliminate tumour progression in mice with intact immune systems. Understanding this type of expression is key to discovering the causes of GBM progression.
First author Jun Yan, Ph.D., a research scientist, showed the FGL2 present in tumour cells controls a specialised group of dendritic cells which activates T-cells. More specifically, FGL2 secreted from tumour cells prevents the differentiation of a special subpopulation of CD103 dendritic cells that are essential for triggering the activation of the tumour-killing T-cells. The study also showed these dendritic cells must find a way to the tumour microenvironment in the central nervous centre (CNS) in order to activate the T cells.
“This study is important because it shows that the immune system must interact in the CNS and in a tumour to be effective. Previously, this interaction was only thought to be necessary for specialised immune organs such as the lymph nodes,” said Amy Heimberger, M.D., professor of Neurosurgery. “It also shows a new mechanism of immune suppression that hasn’t been described before, and it further supports how important FGL2 is to this disease.”
The team also analysed human GBM from The Cancer Genome Atlas and found that lower levels of FGL2 protein expression coupled with high levels of GM-CSF or IFN, DC differentiation inducer or T-cell activator, are associated with longer survival of GBM patients.
Li and Prof Heimberger are actively working on therapeutic strategies to target FGL2.
Findings from the preclinical study have been published in Nature Communications.
Related topics
Immunology, Protein, Proteomics
Related organisations
The University of Texas MD Anderson Cancer Center
Related people
Shulin Li