Researchers grow genetically engineered mini livers to study disease
Posted: 6 August 2019 | Rachael Harper (Drug Target Review) | No comments yet
The first genetically modified mini human livers have been grown in a laboratory, to emulate liver disease progression and test therapeutics.
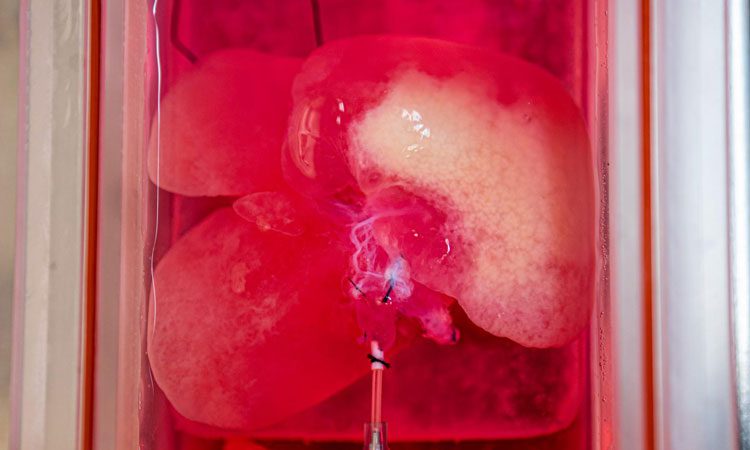
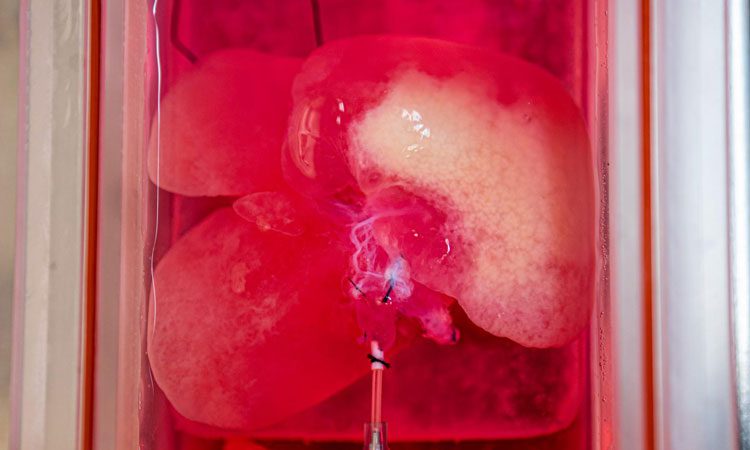
Photograph of rat liver, stripped of rat-specific cells and re-seeded with engineered human liver cells. Photo credit: UPMC
In a new study, researchers at the University of Pittsburgh School of Medicine have chronicled how they transformed genetically engineered human cells into functional, 3D liver tissue that mimics non-alcoholic fatty liver disease (NAFLD).
“This is the first time we can create genetically engineered human mini livers with a disease using stem cells in the lab,” said senior author Alejandro Soto-Gutierrez, MD, PhD, associate professor of pathology at Pitt’s School of Medicine.
This not only aids in understanding the causes of the disease and how it progresses, but also for testing therapeutics.
The researchers exampled the drug Resveratrol in their work, which acts on SIRT1 proteins commonly associated with NAFLD, that was effective in mouse models, but failed in human clinical trials. First, they genetically engineered normal human skin cells to express a chemically activated switch that could tamp down the SIRT1 gene. Then they reprogrammed the cells back to their stem cell state and turned them into liver cells.
After that, they seeded the genetically engineered human liver cells into rat livers stripped of their own cells, where they blossomed into functional 3D mini livers, with blood vessels and other structural features of a normal organ.
That structure is part of what distinguishes mini livers from ‘organoid’ cultures although the mini livers lacked the distinct zones of metabolic function that normal livers have.
Once the mini livers were mature, the researchers flipped the genetic switch to suppress the SIRT1 gene, and the bioengineered mini livers started to mimic the metabolic dysfunction observed in tissues from patients with fatty liver disease.
But just like the clinical trials, Resveratrol wasn’t effective in the lab-grown livers either.
The key, Soto-Gutierrez explained, is that Resveratrol boosts the activity of SIRT1 proteins, not SIRT1 genes. If SIRT1 gene expression is suppressed (like it is in his bioengineered livers, and perhaps also NAFLD patients) there isn’t any protein to act on, so the drug won’t work. It’s targeting the wrong step which is “an insight that could only come from studying functional human tissue”, Soto-Gutierrez said.
“These mini livers aren’t ready for clinical applications like transplantation anytime soon, but I imagine in the future we can make human livers where you can order what kind of function you want, or even enhance function,” he added
The proof-of-concept paper was published in Cell Metabolism.
Related topics
Clinical Trials, Protein, Research & Development, Stem Cells, Targets, Therapeutics
Related conditions
Non-alcoholic fatty liver disease
Related organisations
University of Pittsburgh School of Medicine
Related people
Alejandro Soto-Gutierrez MD PhD