CAR T-cell receptors based on scorpion venom show efficacy in mice
Posted: 5 March 2020 | Victoria Rees (Drug Target Review) | No comments yet
Combining the chlorotoxin peptide with conventional CAR structures, researchers have created a new CAR T cell therapy that has successfully combatted glioblastomas in mice.
Scientists have developed novel anticancer CAR T cells with receptors based on a toxin found in scorpion venom, allowing the cells to recognise and destroy brain tumour cells that often evade immune recognition in mice.
The researchers, from the City of Hope Medical Center and City of Hope Beckman Research Institute, US, found that the new CAR T cells killed glioblastoma tumours in mice without damaging healthy tissues, suggesting the cells could be further developed into a more precisely targeted cell therapy for aggressive brain cancers.
…CTLX binds to a receptor on tumour cells that includes membrane-bound MMP-2″
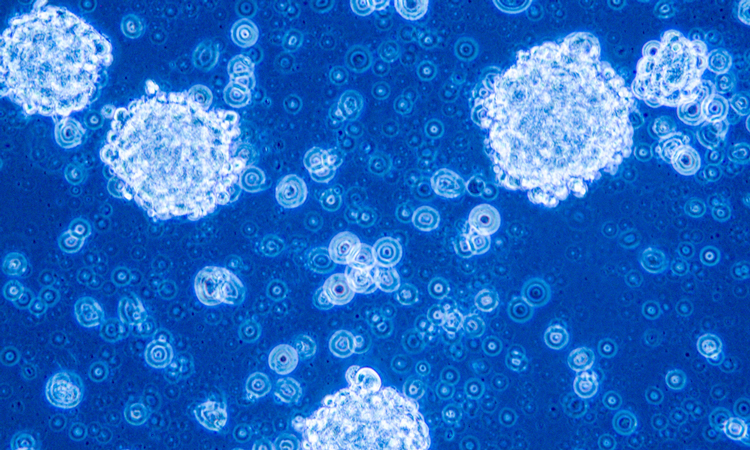
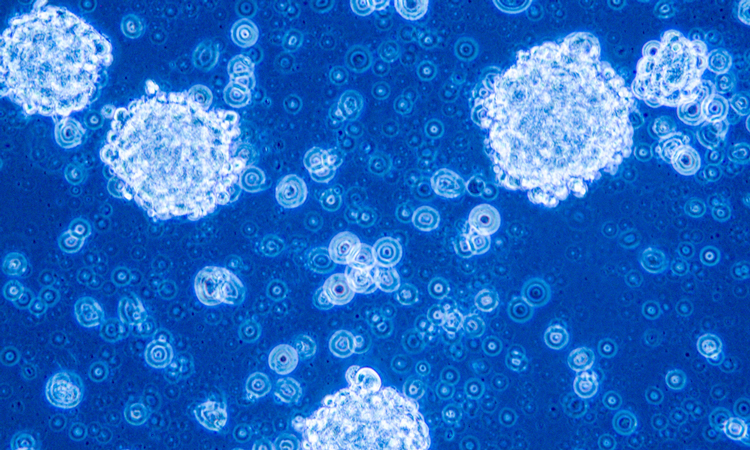
The team were able to overcome the common CAR-T therapy obstacle including glioblastomas changing in response to treatment and severe side effects from CAR T cells attacking non-cancerous cells in organs. They were able to do this by basing their CAR on chlorotoxin – a peptide isolated from the highly venomous death stalker scorpion that is known to bind to glioblastoma cells.
Speaking to Drug Target Review, co-author Dr Christine Brown said: “We used the chlorotoxin peptide (CLTX) as the tumour-targeting domain of the CAR in lieu of the more commonly used antibody-based tumour targeting domains. Specifically, we incorporated the CTLX peptide within a conventional CAR structure that included spacer and transmembrane domains along with the CD28 and CD3-zeta T-cell signalling domains.”
The scientists gave T cells bearing the new CARs to mice with glioblastoma and found the cells eradicated the tumours in many of the animals. The CAR T cells were even effective against tumours that lack some targetable antigens such as the receptor EGFR; they also did not cause adverse reactions or organ damage in the rodents.
Brown explained that for this CAR, CTLX binds to a receptor on tumour cells that includes membrane-bound MMP-2 – this elicits downstream signalling events that activate T-cell killing functions.
She continued that from their work, there are two major findings:
- Broad tumour targeting by CLTX-CAR T cells may be possible. CLTX binds to the majority of patient glioblastoma multiforme tumours and a high proportion of malignant cells within these tumours. The hopes that by broadly targeting the majority of the malignant cells, response rates can be improved and relapse due to antigen escape can be slowed down or inhibited.
- Specific tumour recognition by CLTX-CAR T cells, with no evidence for off-tumour targeting of normal brain or other tissues is also suggested from the results. The researchers did not observe toxicity in CLTX-cross reactive mouse models and off-tumour recognition on a panel of non-malignant human cells was also not observed.
“We believe, taken together, that these results support the potential safety of CLTX-CAR T cells for human testing,” concluded Brown.
The study was published in Science.
Related topics
Drug Targets, Immuno-oncology, Immunotherapy, Oncology, Peptide Therapeutics, Research & Development, Therapeutics
Related conditions
Glioblastoma
Related organisations
City of Hope
Related people
Dr Christine Brown