Novel antibiotic peptide fights ‘superbug’ lung infections in mice
Posted: 4 May 2020 | Victoria Rees (Drug Target Review) | No comments yet
Scientists have developed a new antimicrobial peptide therapy named D8 with high efficacy and low toxicity in mice which could be used to fight lung infections.


Researchers at the University of Pittsburgh Graduate School of Public Health, US, report they have considerably reduced the toxicity of a potential antibiotic, named D8, that fights drug-resistant bacteria, while also improving its stability in fighting infections.
The new antibiotic proved more effective than its experimental predecessor and traditional last-resort antibiotic therapies in fighting drug-resistant bacteria in laboratory cell cultures and mice without notable toxic side-effects, according to the findings.
“We were so surprised and happy,” said lead author Dr Y Peter Di, associate professor in Pitt Public Health’s Department of Environmental and Occupational Health. “At first, we were sceptical and repeated the experiment – but it was 20 times less toxic toward red blood cells in our lab. When we saw similar results in mice, we were really excited.”
The experimental drug that Di’s team developed is built from an engineered cationic antimicrobial peptide (eCAP) which is a synthetic and more efficient version of the naturally occurring antimicrobial peptides that form a first line of defence against infections in humans. eCAPs work by ‘punching into’ bacteria, thereby destroying them.
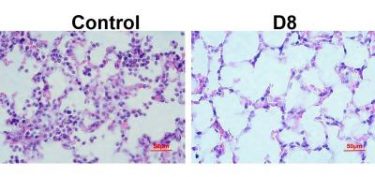
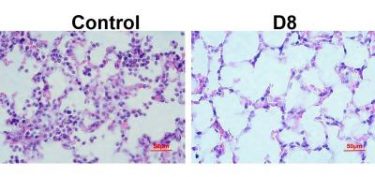
A newly created antibiotic, D8, kills much more drug-resistant bacteria (purple) than the placebo in mouse lungs [credit: B. Deslouches/Pitt].
The team was working with an eCAP called WLBU2, licensed by Pitt’s Peptilogics and entering clinical trials for use in preventing infections associated with knee and hip replacements. They were investigating ways to make WLBU2 more stable so that it stays long enough to fight lingering infections in the lungs.
To defend against foreign invaders, lungs naturally secrete mucus and proteins that also recognise and degrade WLBU2. To navigate this problem, Di’s team constructed a near-mirror image of WLBU2 – which they call ‘D8’ – in hopes it would be less likely to be recognised by the lung’s defences. It worked and at a four-fold lower concentration than WLBU2. The researchers found that D8 eliminated Pseudomonas aeruginosa from blood in the lab.
The team next exposed human red and white blood cells to concentrations of the D8 antibiotic, at nearly 25 times the concentration that would ever be used therapeutically, to see if it would have negative effects on the cells. They found that D8 was considerably less toxic than regular WLBU2, destroying less than one percent of red blood cells and less than 15 percent of white.
The researchers next tested their antibiotic in mice. While WLBU2 at higher than 35μg would kill some mice, there were no fatalities with D8 at four times that concentration.
“This considerable improvement in lowering toxicity, coupled with the new drug’s strong stability and activity against superbugs, is good evidence that this compound will be well-suited for clinical applications in treating respiratory infections,” Di said. However, he also cautioned that they do not know why the new drug is less toxic or how well it is tolerated long-term, so more experimentation is needed before it can be used to treat patients.
The team is exploring its potential use for cystic fibrosis patients whose lives are greatly shortened by drug-resistant lung infections. They also are looking at using it for ventilator-associated pneumonias, which are emerging as serious secondary – and potentially more deadly – infections in COVID-19 patients.
The study was published in Science Advances.
Related topics
Antibiotics, Antimicrobials, Peptide Therapeutics, Research & Development, Therapeutics, Toxicology
Related conditions
Cystic fibrosis
Related organisations
University of Pittsburgh Graduate School of Public Health
Related people
Dr Y Peter Di