Could FDA-approved drug heparin prevent SARS-CoV-2 infection?
Posted: 17 September 2020 | Hannah Balfour (Drug Target Review) | No comments yet
SARS-CoV-2 entry into human cells is dependent on heparan sulfate and disrupting this interaction using heparin reduces infectivity of the coronavirus, find scientists.
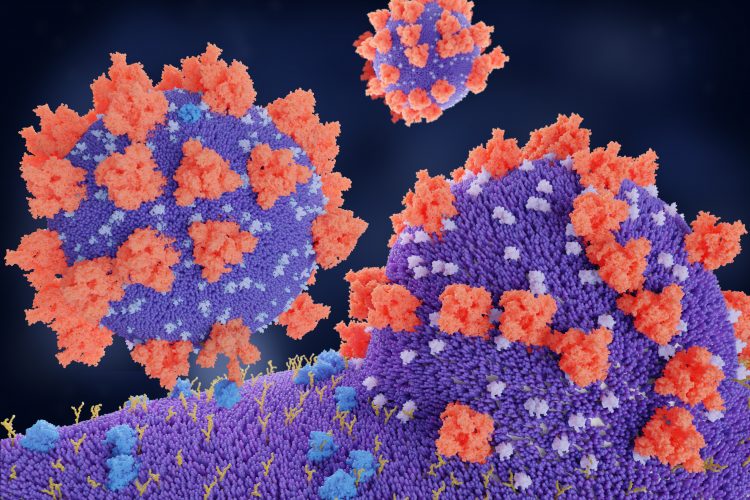
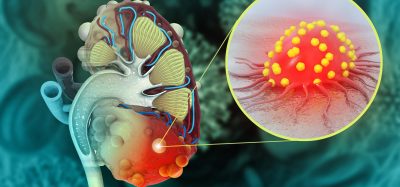
Researchers have identified that in order to enter cells, SARS-CoV-2 – the coronavirus that causes COVID-19 – must bind to both the angiotensin-converting enzyme 2 (ACE2) and heparan sulfate. They demonstrated that blocking this mechanism reduced the ability of SARS-CoV-2 to infect human cells in vitro.
ACE2 was established in January 2020 as the receptor that the Spike (S) protein of SARS-CoV-2 must bind to in order to infect the cells that line the lungs and establish respiratory infections. Preventing this interaction as a means of treating COVID-19 has since become the focus of a huge volume of research.
![SARS-CoV-2 and ACE2 Graphic, University of California San Diego Health Sciences SARS-CoV-2's spike protein must bind both the ACE2 receptor and heparan sulfate to gain entry into human cells [Credit: UC San Diego Health Sciences].](https://www.drugtargetreview.com/wp-content/uploads/SARS-CoV-2-HEPARAN-SULFATE-viral-entry-500x500.jpg)
![SARS-CoV-2 and ACE2 Graphic, University of California San Diego Health Sciences SARS-CoV-2's spike protein must bind both the ACE2 receptor and heparan sulfate to gain entry into human cells [Credit: UC San Diego Health Sciences].](https://www.drugtargetreview.com/wp-content/uploads/SARS-CoV-2-HEPARAN-SULFATE-viral-entry-500x500.jpg)
SARS-CoV-2 and ACE2 Graphic, University of California San Diego Health Sciences
SARS-CoV-2’s spike protein must bind both the ACE2 receptor and heparan sulfate to gain entry into human cells [Credit: UC San Diego Health Sciences].
Scientists at the University of California (UC) San Diego School of Medicine have discovered that the carbohydrate heparan sulfate, also expressed on the surface of lung cells, is a co-receptor for SARS-CoV-2 viral entry. According to their study, published in Cell, without heparan sulfate, SARS-CoV-2 cannot enter human cells.
This finding presents a possible new method for treating COVID-19.
The research, led by Dr Jeffrey Esko, Distinguished Professor of Cellular and Molecular Medicine at UC San Diego School of Medicine and co-director of the Glycobiology Research and Training Center, demonstrated two approaches that reduce the ability of SARS-CoV-2 to infect human cells cultured in vitro: 1) removing heparan sulfate with enzymes or 2) using heparin (a US Food and Drug Administration (FDA)-approved drug formulation of heparan sulfate) as bait to lure and bind the coronavirus away from human cells.
Esko’s team has long studied heparan sulfate and the role it plays in health and disease; however, not necessarily with a focus on viruses. Their experiments were based on a preliminary study which suggested there was an interaction between the coronavirus’s S protein and another carbohydrate related to heparan sulfate. They began testing their theories in the lab and discovered that the receptor binding domain (RBD) of the SARS-CoV-2 S protein binds to heparin. When heparin is bound, the RBD opens up and the result is increased binding to ACE2. The virus, they found, must bind both heparan sulfate and ACE2 on the cell surface in order to enter human lung in vitro.
Once this mechanism of entry was established, they sought to disrupt it. In their study, enzymes that remove heparan sulfate from cell surfaces prevented SARS-CoV-2 from entering cells. Likewise, treatment with heparin also blocked infection by up to 80 to 90 percent. The heparin treatment worked as an anti-viral at doses currently given to patients, even when the researchers removed the anticoagulant region of the protein.
Esko cautioned that the findings are still far from translating into a COVID-19 treatment for people, heparin and heparan sulfate inhibitors would have to be tested in animal models of SARS-CoV-2 infection prior to translation into humans. said Esko.
He concluded: “This is one of the most exciting periods of my career – all of the things we have learned about heparan sulfate and the resources we have developed over the years have come together with a variety of experts across multiple institutions who were quick to collaborate and share ideas. If there is a silver lining to this pandemic, I hope it is that the scientific community will continue to work rapidly together like this to address other problems.”
Related topics
Cell-based assays, Disease Research, Drug Repurposing, Drug Targets, Immunology, In Vitro, Therapeutics
Related conditions
Coronavirus, Covid-19
Related organisations
University of California (UC) San Diego School of Medicine
Related people
Dr Jeffrey Esko