Lung and brain organoids respond differently to SARS-CoV-2 infection in lab
Posted: 25 February 2021 | Victoria Rees (Drug Target Review) | No comments yet
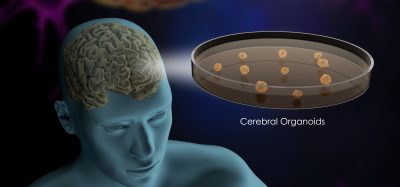
Researchers have developed stem cell-derived organoids to reveal how SARS-CoV-2 interacts with lung and brain cells differently.
Researchers at the University of California (UC) San Diego School of Medicine, US, have used stem cell-derived organoids to study how SARS-CoV-2 interacts with various organ systems and develop therapies to block infection.
“We are finding that SARS-CoV-2 does not infect the entire body in the same way,” said Professor Tariq Rana, one of the lead researchers of the study. “In different cell types, the virus triggers the expression of different genes and we see different outcomes.”
According to the team, their lung and brain organoids produce the molecules angiotensin-converting enzyme 2 (ACE2) and TMPRSS2, which sit on the outer surfaces of cells. SARS-CoV-2 binds to these molecules with its Spike (S) protein as a means to enter cells and establish infection.
The team developed a pseudovirus – a non-infectious version of SARS-CoV-2 – and labelled it with green fluorescent protein (GFP). The fluorescent label allowed them to quantify the binding of the virus’ S protein to ACE2 receptors in human lung and brain organoids and evaluate the cells’ responses.
The team observed approximately 10-fold more ACE2 and TMPRSS2 receptors and correspondingly much higher viral infection in lung organoids, as compared to brain organoids. Treatment with viral S protein or TMPRSS2 inhibitors reduced infection levels in both organoids.
“We saw dots of fluorescence in the brain organoids, but it was the lung organoids that really lit up,” Rana said.
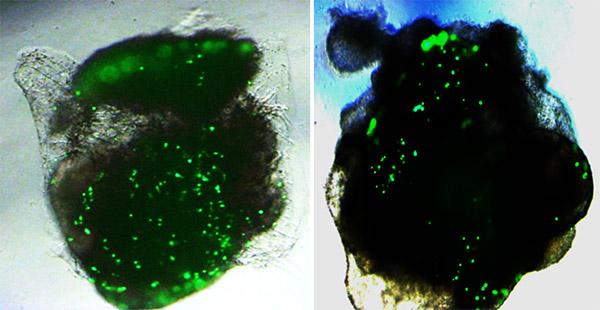
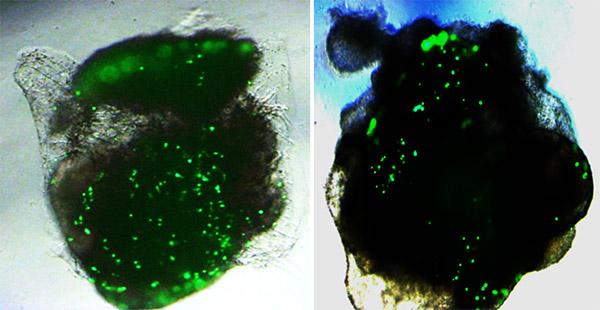
UC San Diego School of Medicine researchers found approximately 10-fold higher SARS-CoV-2 infection (green) in lung organoids (left), compared to brain organoids (right) [credit: UC San Diego Health Sciences].
Besides differences in infectivity levels, the researchers found that the lung and brain organoids also differed in their responses to the virus. SARS-CoV-2-infected lung organoids pumped out molecules intended to summon help from the immune system – interferons, cytokines and chemokines. Infected brain organoids, on the other hand, increased their production of other molecules, such as TLR3, a member of the toll-like receptor family that plays a fundamental role in pathogen recognition and activation of innate immunity.
Rana explained that, while it might seem at first like the brain organoid reaction is just another form of immune response, those molecules can also aid in programmed cell death.
“The way we are seeing brain cells react to the virus may help explain some of the neurological effects reported by patients with COVID-19,” Rana said. “In animals over-expressing ACE2 receptors, you see everything light up with infection, even the brain, so everyone thinks this is the real situation. However, we found that is likely not the case.”
The team additionally validated their findings by applying live, infectious SARS-CoV-2 to lung and brain organoids.
The researchers are now developing SARS-CoV-2 inhibitors and testing how well they work in organoid models derived from people of a variety of racial and ethnic backgrounds.
The findings are published in Stem Cell Reports.
Related topics
Disease Research, Immunology, Organoids, Stem Cells
Related conditions
Covid-19
Related organisations
University of California San Diego School of Medicine
Related people
Professor Tariq Rana