Nanodecoy therapy neutralises SARS-CoV-2 in macaques
Posted: 18 June 2021 | Victoria Rees (Drug Target Review) | No comments yet
Lung spheroid cells can act as nanodecoys for the SARS-CoV-2 Spike protein to bind to, according to a new pre-clinical study.
Nanodecoys made from human lung spheroid cells (LSCs) can bind to and neutralise SARS-CoV-2, promoting viral clearance and reducing lung injury in a macaque model of COVID-19. The study was conducted at North Carolina State University, US, and the researchers found that by mimicking the receptor that the virus binds to rather than targeting the virus itself, nanodecoy therapy could remain effective against emerging variants of the virus.
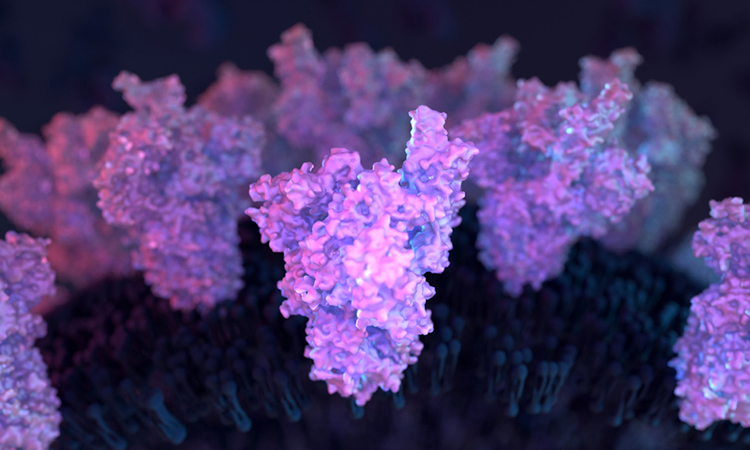
According to the team, SARS-CoV-2 enters a cell when its Spike (S) protein binds to the angiotensin-converting enzyme 2 (ACE2) receptor on the cell’s surface. LSCs – a natural mixture of lung epithelial stem cells and mesenchymal cells – also express ACE2, making them a perfect vehicle for tricking the virus.
“If you think of the S protein as a key and the cell’s ACE2 receptor as a lock, then what we are doing with the nanodecoys is overwhelming the virus with fake locks so that it cannot find the ones that let it enter lung cells,” said Professor Ke Cheng, corresponding author of the research. “The fake locks bind and trap the virus, preventing it from infecting cells and replicating and the body’s immune system takes care of the rest.”
The researchers converted individual LSCs into nanovesicles with ACE2 receptors and other lung cell-specific proteins on the surface.
They confirmed that the S protein bound to the ACE2 receptors on the decoys in vitro, then used a fabricated SARS-CoV-2 mimic virus for in vivo testing in a mouse model. The decoys were delivered via inhalation therapy. In mice, the nanodecoys remained in the lungs for 72 hours after one dose and accelerated clearance of the mimic virus.
Finally, a contract research organisation conducted a pilot study in a macaque model and found that inhalation therapy with the nanodecoys accelerated viral clearance and reduced inflammation and fibrosis in the lungs. Although no toxicity was noted in either the mouse or macaque study, the team note that further study will be necessary to translate this therapy for human testing and determine exactly how the nanodecoys are cleared by the body.
“These nanodecoys are essentially cell ‘ghosts’ and one LSC can generate around 11,000 of them,” Cheng said. “Deploying millions of these decoys exponentially increases the surface area of fake binding sites for trapping the virus and their small size basically turns them into little bite-sized snacks for macrophages, so they are cleared very efficiently.”
The researchers point out three other benefits of the LSC nanodecoys. First, they can be delivered non-invasively to the lungs via inhalation therapy. Second, since the nanodecoys are acellular, they can be easily preserved and remain stable longer, enabling off-the-shelf use. Finally, LSCs are already in use in other clinical trials, so there is an increased likelihood of being able to use them in the near future.
The research is published in Nature Nanotechnology.
Related topics
In Vivo, Molecular Targets, Pharmacology, Stem Cells, Target Validation, Translational Science
Related conditions
Covid-19
Related organisations
North Carolina State University
Related people
Professor Ke Cheng