Stem cell therapy repairs injured peripheral nerves in animal models
Posted: 12 October 2021 | Anna Begley (Drug Target Review) | No comments yet
Gingiva-derived mesenchymal stem cells were used to surgically repair injured peripheral nerves, showing potential for new therapies.
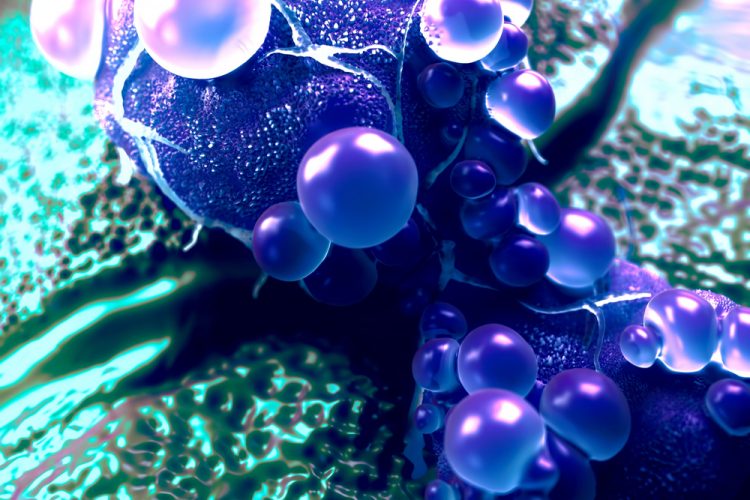
Researchers from the University of Pennsylvania, US, have demonstrated the use of coaxed human gingiva-derived mesenchymal stem cells (GMSCs) in repairing peripheral nerves in animal models. According to the team, their findings could lead to clinical applications for human nerve repair in the future.
Currently, faced with repairing a major nerve injury to the face or mouth, surgeons can take a nerve from an arm or leg and use to it restore movement or sensation to the original site of trauma. This approach, known as a nerve autograft, is the standard of care for nerve repair. However, it can take a toll on a previously uninjured body part and the procedure does not always result in complete and functional nerve regrowth.
ARTICLE: “Noisy” gene expression may help improve stem cell therapies
DISCOVER MORE HERE
In an innovative approach to guided nerve repair, detailed in npj Regenerative Medicine, the team coaxed human gingiva-derived mesenchymal stem cells (GMSCs) to grow Schwann-like cells, the pro-regenerative cells of the peripheral nervous system that make myelin and neural growth factors. They demonstrated that infusing a scaffold with these cells and using them to guide the repair of facial nerve injuries in an animal model had the same effectiveness as an autograft procedure.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
“Instead of an autograft, which causes unnecessary morbidity, we wanted to create a biological approach and use the regenerating ability of stem cells,” explained senior author Professor Ahn Le. “To be able to recreate nerve cells in this way is really a new paradigm.”
The researchers grew the GMSCs in a collagen matrix using specific conditions that encouraged the cells to grow more like Schwann cells, with the cells’ identity confirmed with a variety of genetic markers. “We observed this very interesting phenomenon that when we changed that matrix density and suspended the cells three-dimensionally, they changed to have more neural crest properties, like Schwann cells,” Le added.
Using commercially available scaffolds for nerve growth, the researchers introduced the cells into collagen hydrogel. “The cells migrate into the nerve graft and create a sheet of Schwann cells,” continued Le. “By doing so they are forming the functionalised nerve guidance to guide axon generation in the gap left by an injury.”
When the team implanted these grafts into rodents with a facial nerve injury and then tested the results, they saw evidence of a functional repair. The animals had less facial droop than those that received an “empty” graft and nerve conduction was restored. The implanted stem cells also survived in the animals for months following the transplant.
While the current study worked at repairing a small gap in a nerve, the researchers aim to continue refining the method to try to repair larger gaps, as often arise when oral cancer necessitates surgical removal of a tumour.
Le noted that this approach would also give patients with oral cancer or facial trauma the opportunity to use their own tissue to recover motor function and sensation and to have cosmetic improvements following a repair. Moreover, while Le’s group focuses on the head and neck, further work on this model could translate to nerve repair in other areas of the body.
Related topics
In Vivo, Molecular Biology, Oncology, Regenerative Medicine, Small Molecules, Stem Cells, Therapeutics
Related conditions
nerve damage
Related organisations
Pennsylvania University
Related people
Professor Ahn Le